The birth of a child is a joyful event that changes life. However, for many women, this period can be overshadowed by unexpected emotional difficulties. Postpartum depression is a serious condition affecting numerous young mothers. In this article, I will discuss all aspects of postpartum depression to help you cope with it.

What is Postpartum Depression?
Postpartum Depression (PPD) is a form of clinical depression that can occur within the first year after childbirth. It is a severe mood disorder that affects a woman’s physical and emotional state, as well as her ability to care for herself and her newborn. Postpartum depression is characterized by deep sadness, anxiety, and a sense of emptiness that does not pass on its own over time.
Despite the prevalence of PPD, many women feel ashamed to talk about their feelings, fearing judgment or misunderstanding. It is important to remember that postpartum depression is not a sign of weakness or an inability to be a good mother but a medical condition requiring professional help and support.
Postpartum depression is not uncommon. According to the World Health Organization, 10% to 20% of women experience depression during pregnancy or the postpartum period. In some countries, this rate may reach 40%. These numbers highlight the importance of discussing PPD and raising awareness of this issue.
Early detection and treatment of postpartum depression are crucial for the health of both mother and child. Unfortunately, many women do not receive the necessary assistance due to the stigma around mental disorders or lack of awareness of PPD symptoms.

Symptoms of Postpartum Depression
The emotional manifestations of PPD can range from mild sadness to deep despair. Many women experience an inexplicable sense of guilt, considering themselves “bad mothers” because of their condition. These negative emotions may be exacerbated by the physical exhaustion associated with caring for a newborn.
It is essential to note that some symptoms of PPD may be mistakenly attributed to normal postpartum consequences and the adjustment to motherhood. However, the key difference lies in their intensity and duration. If negative feelings persist for several weeks or months, professional help should be sought.
Postpartum depression can present in various ways, and PPD symptoms often develop gradually, making it difficult for the woman herself and her loved ones to recognize them in time. Nevertheless, there are common signs that are essential to recognize.
Emotional Symptoms
Emotional symptoms of PPD may include:
- persistent feelings of sadness or emptiness;
- loss of interest in previously enjoyable activities;
- feelings of hopelessness or helplessness;
- severe anxiety or panic attacks;
- irritability and anger outbursts;
- feelings of guilt or inadequacy;
- difficulty making decisions;
- thoughts of harming oneself or the baby.
Physical Symptoms
PPD can also manifest physically:
- sleep disturbances (insomnia or excessive sleepiness);
- appetite changes (loss of appetite or overeating);
- chronic fatigue and lack of energy;
- physical pains without an obvious cause (headaches, muscle aches);
- problems with concentration and memory.
Behavioral Changes
Postpartum depression may lead to noticeable behavioral changes:
- social isolation, withdrawal from family and friends;
- difficulty bonding with the baby;
- neglect of personal hygiene;
- procrastination and trouble completing daily tasks;
- substance abuse (alcohol or other substances).
Difference from “Baby Blues”
The “baby blues” is a temporary state of emotional downturn, anxiety, and tearfulness experienced by about 80% of women in the first days after childbirth. This state typically lasts from a few days to two weeks and is associated with hormonal changes, fatigue, and adjustment to a new lifestyle.
Unlike postpartum depression, the baby blues is less intense and resolves independently without special treatment, while PPD is a more serious and prolonged condition that requires professional help.

Risk Factors for Postpartum Depression
Postpartum depression does not select its victims randomly. A number of factors can increase the likelihood of this condition developing in a new mother. Understanding these risk factors helps in early detection and prevention of PPD.
The biological changes occurring in a woman’s body after childbirth play a significant role in the development of PPD. The sharp drop in hormone levels, especially estrogen and progesterone, can cause severe mood swings. Changes in thyroid function can also contribute to depressive symptoms.
Additionally, psychological and social factors are of great importance. Stressful life events, financial difficulties, relationship problems, or a lack of support from loved ones can significantly increase the risk of developing PPD. It is important to note that having risk factors does not mean that depression will inevitably develop but requires increased attention to the woman’s emotional state during the postpartum period.
Hormonal Changes
The sudden drop in estrogen and progesterone levels after childbirth can cause significant mood changes. In addition, changes in thyroid hormone levels can lead to depression-like symptoms.
Personal or Family History of Depression
Women who have previously suffered from depression or other mental disorders are at a higher risk of developing PPD. The risk also increases if there is a family history of depression or bipolar disorder.
Stressful Life Events
Stressful events during pregnancy or soon after childbirth can increase the risk of PPD. These include:
- complications during pregnancy or childbirth;
- financial difficulties;
- relationship problems;
- the death of a loved one;
- moving or changing jobs.
Lack of Support
A lack of emotional or practical support from a partner, family, or friends can significantly increase the risk of postpartum depression.

The Impact of Postpartum Depression on Mother and Child
Postpartum depression is not only a personal problem for the mother but also a condition that can profoundly affect the entire family, especially the newborn. Understanding the scale of this impact is crucial for recognizing the importance of timely treatment and support.
For the mother, PPD can become a source of deep emotional suffering, preventing her from enjoying motherhood and fully caring for her child. Women with PPD often experience difficulty forming an emotional connection with their infant, which may cause feelings of guilt and worsen the depressive state.
The impact on the child can be no less serious. Studies show that children of mothers suffering from untreated postpartum depression often experience delays in cognitive and emotional development. These effects can manifest not only in infancy but also later in life, affecting the child’s social skills and academic achievements.
Consequences for the Mother’s Health
Postpartum depression can lead to:
- chronic depression;
- sleep and eating problems;
- an increased risk of other mental disorders;
- difficulties in performing daily tasks;
- social isolation;
- in severe cases, suicidal thoughts.
Impact on Child Development
Children of mothers with untreated PPD may experience:
- delays in cognitive and emotional development;
- attachment issues;
- an increased risk of behavioral problems in the future;
- difficulties with social interactions;
- an increased risk of developing depression during adolescence.
Impact on Family Relationships
Postpartum depression can negatively affect:
- relationships with the partner;
- bonding between mother and child;
- the overall family atmosphere;
- the ability to handle parental responsibilities.

Diagnosis of Postpartum Depression
Timely and accurate diagnosis of postpartum depression (PPD) plays a crucial role in effective treatment and preventing long-term consequences for both mother and child. However, identifying PPD can be challenging due to the stigma surrounding mental health disorders and the reluctance of women to acknowledge the issue.
The process of diagnosing PPD typically begins with a thorough medical history and symptom assessment. Doctors and psychologists use specialized questionnaires, such as the Edinburgh Postnatal Depression Scale, to evaluate the severity of symptoms and the risk of more serious mental health problems.
It’s essential to understand that diagnosing PPD is not merely a formal questionnaire process. It is an opportunity for women to openly and without judgment discuss their feelings and fears in a safe environment. A well-conducted diagnosis can be the first step toward recovery and returning to the joy of motherhood.
When to See a Doctor?
You should consult a doctor if:
- depressive symptoms last for more than two weeks;
- symptoms interfere with daily responsibilities;
- there are thoughts of self-harm or harming the baby;
- there is a feeling of being unable to care for the baby.
Assessment Methods
Various methods are used for diagnosing PPD:
- Questionnaires (e.g., the Edinburgh Postnatal Depression Scale);
- Clinical interview with a psychiatrist or psychologist;
- Physical examination to rule out other medical causes of symptoms.
Treatment Methods for Postpartum Depression
Treating postpartum depression is a complex process that requires an individualized approach for each patient. Modern medicine offers several effective methods that can help women overcome this challenging condition and return to a fulfilling life.
Psychotherapy is one of the cornerstones of PPD treatment. Cognitive-behavioral therapy (CBT) and interpersonal therapy have shown particular effectiveness in treating postpartum depression. These approaches help women reframe negative beliefs, improve problem-solving skills, and strengthen social connections.
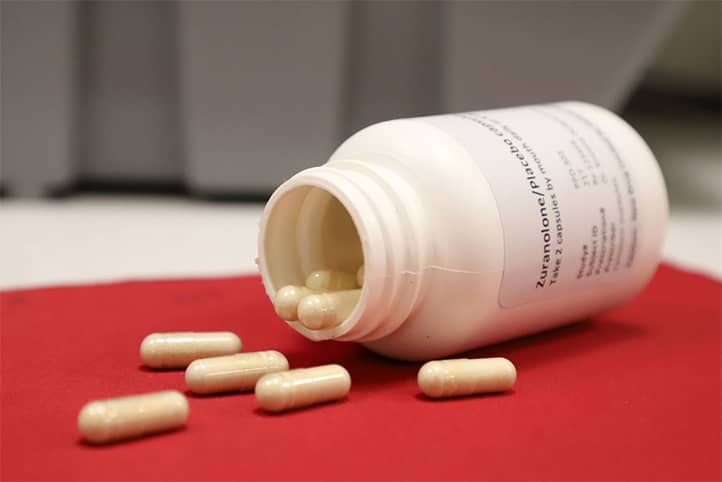
In some cases, medication may be recommended, especially for severe forms of PPD. Modern antidepressants, chosen to account for the individual characteristics of the patient and the possibility of breastfeeding, can significantly ease depressive symptoms and help women return to normal life more quickly.
Psychotherapy
The most effective types of therapy for PPD include:
- Cognitive-behavioral therapy (CBT) helps identify and change negative thoughts and behaviors. The therapist works with the patient on developing problem-solving and coping strategies.
- Interpersonal therapy focuses on improving relationships and social support. It aids in resolving conflicts and improving communication with loved ones.
Medication
In some cases, a doctor may prescribe antidepressants. It’s essential to discuss all risks and benefits of medication treatment with a doctor, especially if the woman is breastfeeding.
Alternative Methods
Additional methods that may help in treating PPD include:
- light therapy (especially effective for seasonal depression);
- regular physical exercise;
- relaxation and meditation techniques;
- acupuncture.

Prevention and Self-Care for Postpartum Depression
Preventing postpartum depression begins well before the child’s birth and continues throughout the postpartum period. Awareness of the risk factors and symptoms of PPD allows women and their loved ones to be better prepared for potential emotional challenges.
Self-care plays a crucial role in the prevention and management of PPD. Regular physical activity, a healthy diet, and adequate sleep can significantly improve a young mother’s emotional well-being. It is also important to find time for rest and enjoyable activities, even in the demanding schedule of caring for a newborn.
Building a support network is another key aspect of PPD prevention. This may include connecting with other new mothers, participating in support groups, or regularly talking with close people about one’s experiences. Openly discussing emotional challenges helps reduce feelings of isolation and boost self-confidence as a mother.
Preparing for Birth and Motherhood
- Attending parenting classes;
- Discussing expectations and fears with a partner and doctor;
- Planning postpartum support.
The Importance of Sleep and Rest
- Trying to sleep when the baby sleeps;
- Sharing night duties with a partner;
- Accepting help from family and friends to ensure adequate rest.
Balanced Nutrition
- Regular, balanced meals;
- Including foods rich in omega-3 fatty acids in the diet;
- Limiting caffeine and alcohol.
Physical Activity
- Regular, moderate exercise (after doctor approval);
- Walking outdoors with the baby;
- Engaging in yoga or other relaxing activities.
Social Support
- Maintaining contact with friends and family;
- Joining support groups for new mothers;
- Discussing feelings with trusted people.

The Role of Family Support in Postpartum Depression
The support of loved ones plays a significant role in overcoming postpartum depression. A partner, family, and friends can be a reliable source of support for a woman going through this challenging time. Their understanding and involvement can greatly accelerate recovery.
It’s important for loved ones to be informed about the symptoms and characteristics of PPD. This will help them recognize the signs of depression and provide the necessary assistance. Active listening without judgment, emotional support, and practical help in caring for the baby are invaluable contributions to the fight against PPD.
Loved ones can also play a crucial role in encouraging women to seek professional help when needed. Sometimes the persistence of a partner or family members becomes the deciding factor for beginning PPD treatment.
How to Recognize Signs of Depression in a Woman?
Loved ones should pay attention to the following signs:
- Persistent sadness or irritability;
- Loss of interest in the baby or daily activities;
- Significant changes in appetite or weight;
- Sleep problems not related to baby care;
- Expressions of guilt or worthlessness.
Ways to Provide Emotional and Practical Support
Partners and family members can help in the following ways:
- Active listening without judgment;
- Helping with baby care and household chores;
- Encouraging rest and self-care;
- Accompanying to doctor’s appointments;
- Expressing love and support.
When to Insist on Seeking Professional Help?
It is necessary to insist on consulting a specialist if:
- Symptoms do not improve over time;
- Postpartum depression interferes with daily life and baby care;
- Thoughts of self-harm or harming the baby arise.

Resources and Support for Women with Postpartum Depression
In today’s world, there are numerous resources available for women suffering from postpartum depression (PPD). Awareness of these resources and the ability to use them can be crucial to successfully overcoming PPD.
Support groups, both online and offline, provide a unique opportunity for sharing experiences and receiving emotional support from other women who have faced similar challenges. These groups can be a source of valuable practical advice and a sense of community, which is so essential during the struggle with PPD.
Online resources, including specialized websites and forums, offer extensive information on postpartum depression, treatment methods, and self-help strategies. However, it is important to approach online resources critically, prioritizing reliable sources and professional consultations.
Support Groups for New Mothers
Support groups provide an opportunity to:
- communicate with other moms experiencing similar challenges;
- receive emotional support;
- exchange practical advice on childcare.
Online Resources and Forums
Internet resources can be useful for:
- obtaining information on postpartum depression;
- participating in online forums and support groups;
- accessing educational materials on motherhood and mental health.
Crisis Center Contacts and Specialists
It is important to have access to:
- hotlines for emergency psychological assistance;
- contacts of local psychologists and psychiatrists specializing in postpartum depression;
- information on nearby medical institutions providing help with PPD.

Myths and Facts about Postpartum Depression
Postpartum depression is surrounded by many myths and misconceptions that prevent women from recognizing the issue and seeking help. Debunking these myths is an important step in combating PPD stigma and improving the quality of support for young mothers.
One of the most harmful myths is that postpartum depression is simply a “weakness of character” or an inability to cope with maternal responsibilities. In reality, PPD is a serious medical condition caused by the complex interplay of biological, psychological, and social factors.
Another common misconception is the belief that postpartum depression always appears immediately after childbirth and resolves on its own. In reality, symptoms can appear at any time within the first year after childbirth, and without proper treatment, PPD can last for months or even years.
Myth 1: Postpartum depression is just “baby blues”
- Fact: Although “baby blues” and PPD have similar symptoms, postpartum depression is a serious condition that lasts longer and requires professional treatment.
Myth 2: If you have PPD, you’re a bad mother
- Fact: Postpartum depression is a medical condition, unrelated to maternal qualities. Many excellent mothers suffer from PPD.
Myth 3: Postpartum depression will go away on its own if you wait
- Fact: Without treatment, PPD can last for months or even years, negatively impacting the mother’s health and the child’s development.
Myth 4: Taking medication for PPD is dangerous for the baby while breastfeeding
- Fact: There are antidepressants that are safe for breastfeeding. A doctor can choose the right treatment.
Myth 5: Postpartum depression starts right after childbirth
- Fact: PPD can develop at any time within the first year after childbirth and sometimes later.

Recovery Stories: Experiences of Women Who Overcame PPD
Real stories of women who have successfully overcome postpartum depression can inspire and provide hope for those currently struggling with the condition. These stories show that recovery is possible and that after the dark period of PPD, it is possible to rediscover the joy of motherhood.
Each recovery story is unique, but common themes often emerge: the importance of seeking help on time, the role of support from loved ones, and the effectiveness of proper treatment. Many women note that overcoming PPD made them stronger and helped them understand themselves better.
The experiences of women who have gone through PPD also highlight the importance of openly discussing emotional difficulties in the postpartum period. Many who share their stories speak about their desire to help other mothers in similar situations and to contribute to fighting the stigma around postpartum depression.
Anna’s Story: From Despair to the Joy of Motherhood
Anna, 28 years old, mother of two, shares: “After the birth of my first child, I felt empty and guilty. I couldn’t enjoy motherhood as I expected. Seeking help, I underwent psychotherapy and found support in a group for young mothers. Now I enjoy every moment with my children and know that I can handle any challenge.”
Maria’s Experience: When Support Makes All the Difference
Maria, 35, says: “My husband was the first to notice my symptoms of depression. Thanks to his persistence, I sought help from a psychologist. A combination of therapy and family support helped me through the toughest period. Now I understand how important it is to speak up about your problems.”
Elena’s Path: From PPD to Helping Others
Elena, 42, shares her experience: “After overcoming postpartum depression, I decided to become a consultant for young mothers. My experience helps me support other women going through this ordeal. It’s important to remember that recovery is possible and that you are not alone in this fight.”

The Role of a Partner in Overcoming Postpartum Depression
A partner plays a crucial role in the fight against postpartum depression, often becoming the first line of support for the new mother. Recognizing the importance of this role can significantly impact recovery and the overall well-being of the family during this challenging time.
Emotional support from a partner is invaluable. The ability to listen without judgment, show empathy, and be patient allows the woman to feel less isolated and more understood in her experiences. The partner can be a reliable anchor, helping to navigate the emotional storm that characterizes PPD.
Practical support is also essential. Active involvement in childcare, taking on household chores, and ensuring the young mother has time to rest significantly reduce stress levels and contribute to a quicker recovery. The partner can also act as a liaison with medical professionals, helping to organize and support the treatment process.
Emotional Support
- Be patient and understanding.
- Listen without judgment.
- Regularly express love and support.
Practical Assistance
- Actively participate in childcare.
- Take on household chores.
- Provide the mother with time to rest and sleep.
Encouraging Treatment
- Accompany her to doctor’s appointments.
- Help in following the treatment plan.
- Be ready to seek emergency help if needed.

Postpartum Depression and Career: Finding Balance
Returning to work after childbirth is challenging for any woman, but for those dealing with postpartum depression, this process can be especially difficult. Finding a balance between professional responsibilities and motherhood in the context of PPD requires special attention and a strategic approach.
Open communication with the employer about one’s condition, if possible, can help create a more supportive work environment. Many companies today offer flexible work schedules or the option to work remotely, which significantly eases the transition back to the professional sphere for new mothers.
It is essential to remember that recovery from PPD is a process, and it’s unrealistic to expect an immediate return to previous performance levels. Gradually increasing workload, taking regular breaks for rest and self-care, and maintaining ongoing communication with colleagues and supervisors will make this transition smoother and less stressful.
Planning the Return to Work
- Discuss a gradual return with your employer.
- Consider part-time or remote work options.
- Arrange reliable childcare in advance.
Managing Stress at Work
- Set realistic expectations for yourself.
- Practice stress management techniques (diaphragmatic breathing, meditation).
- Don’t hesitate to ask colleagues for help if needed.
Balancing Work and Personal Life
- Set clear boundaries between work and home.
- Schedule time for self-care and rest.
- Maintain open communication with your partner about the division of responsibilities.

Postpartum Depression in Fathers: An Overlooked Issue
While postpartum depression is more commonly associated with women, more research shows that men can also suffer from this condition. Recognizing and understanding postpartum depression in fathers is an important step toward ensuring the well-being of the entire family during the postnatal period.
Symptoms of PPD in fathers may differ from those observed in mothers. Men are more likely to display irritability, aggression, or immerse themselves in work rather than openly expressing sadness or anxiety. These differences in manifestations can make it difficult for both men and their loved ones to identify the issue.
Risk factors for developing PPD in fathers include stress related to new parenting responsibilities, financial difficulties, changes in relationships with their partners, and the presence of postpartum depression in the mother. Raising awareness about this issue and encouraging men to seek help if they experience emotional difficulties after the birth of a child is essential.
Symptoms of Postpartum Depression in Men
- Irritability and outbursts of anger;
- Detachment from family and friends;
- Increased anxiety;
- Changes in sleep and appetite;
- Substance abuse.
Risk Factors
- Partner’s postpartum depression;
- Financial stress;
- Lack of support;
- Personal history of depression.
Importance of Seeking Help
Men often hesitate to seek help due to stigma. It’s important to remember that treating postpartum depression in fathers is just as crucial for the family’s well-being.

Conclusion
Postpartum depression is a serious condition that affects many women and their families during the postnatal period. Understanding the nature of PPD, its symptoms, and treatment methods is essential for ensuring the health and well-being of young mothers and their children.
It’s crucial to remember that postpartum depression is not a sign of weakness or failure in motherhood. It’s a medical condition that requires professional assistance.
The support of loved ones plays a key role in overcoming PPD. Partners, family, and friends can provide invaluable help by offering emotional support and practical assistance. Open discussion of emotional difficulties in the postnatal period reduces the stigma surrounding PPD and encourages women to seek help.
Prevention and self-care also play a role in the fight against postpartum depression. Taking care of physical health, getting regular rest, and maintaining social connections significantly improve a young mother’s emotional well-being. Participation in support groups and utilizing available resources help women feel less isolated and more confident in your role as a mother.
Research into PPD continues to advance, opening new avenues for diagnosis and treatment of this condition. Innovative approaches such as personalized hormone therapy and neuromodulation techniques offer hope for more effective treatment of PPD in the future.
In conclusion, it is important to emphasize that postpartum depression is a surmountable condition. With proper treatment and support, women can fully recover and enjoy the joys of motherhood. Raising awareness of PPD, combating stigma, and ensuring access to quality care are key steps to improving the health and well-being of new mothers and their families.




