Compulsive Overeating is not just occasional episodes of “overindulgence,” but a serious eating disorder in which a person regularly experiences uncontrollable binge-eating episodes accompanied by feelings of shame and helplessness. Unlike situational overeating (for example, at a holiday table), compulsive overeating occurs independently of actual hunger and most often serves as a way to suppress stress, anxiety, or other difficult emotions.
The main danger of compulsive overeating lies in its destructive impact on both physical health and mental well-being. Excess weight, digestive issues, diabetes, and cardiovascular diseases are just some of the possible consequences. But emotional state suffers no less: feelings of guilt after breakdowns, self-loathing, and a sense of losing control create a vicious cycle that is difficult to break.
This problem requires careful attention because many people live with compulsive overeating for years without even realizing that their “lack of willpower” is actually a psychological response to deeper issues.

What is Compulsive Overeating?
Compulsive overeating is not just a bad habit or a lack of willpower. It is a serious eating disorder recognized by the medical community as a distinct condition. If you’ve ever felt unable to stop eating even when full or noticed that food becomes a way to cope with stress—you may have experienced manifestations of this disorder.
The key difference between compulsive overeating and simply “overdoing it at dinner” lies in its regularity and emotional underpinnings. These are not isolated incidents but a recurring behavioral pattern that significantly impacts quality of life. Let’s explore how to recognize this disorder, how it differs from other eating disorders, and who is at risk.
Key Signs
Compulsive overeating has several characteristic symptoms that distinguish it from ordinary overeating:
- Uncontrollable binge episodes. A person consumes a large amount of food in a short period (e.g., 1–2 hours) and feels unable to stop, even when physically uncomfortable.
- Absence of physical hunger. Binge episodes often occur not due to the body’s need for energy but in response to emotional states—stress, boredom, anxiety, or depression.
- Feelings of guilt and shame. After an overeating episode, the person experiences intense negative emotions, ranging from frustration to deep remorse. Unlike bulimia, compulsive overeating typically does not involve attempts to “purge” (through vomiting, laxatives, or excessive exercise).
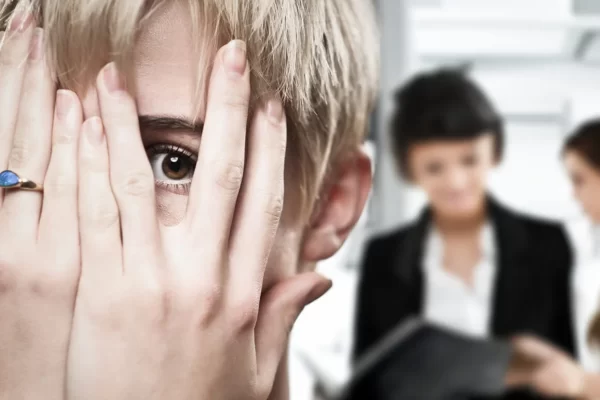
- Secrecy. Many people with this disorder eat in secret, ashamed of their behavior, and avoid discussing the issue even with loved ones.
- Absence of compensatory behavior. Unlike bulimia, compulsive overeating does not involve attempts to “compensate” for the food consumed—for example, by inducing vomiting or fasting the next day.
These signs occur not occasionally but regularly—at least once a week for several months.
Differences from Bulimia and Anorexia
Compulsive overeating is often confused with other eating disorders, but it has fundamental differences:
- Bulimia involves alternating episodes of binge eating and “purging” (vomiting, laxatives, fasting). Compulsive overeating does not include such behavior.
- Anorexia is characterized by deliberate food restriction, fear of weight gain, and distorted body image. People with anorexia may occasionally overeat but then compensate severely through fasting or excessive exercise. Compulsive overeating lacks this cyclical pattern.
Simply put: if a person with bulimia tries to “get rid” of what they’ve eaten, and a person with anorexia controls every bite, then someone with compulsive overeating simply eats without stopping but does not take active steps to “correct” the consequences.
Statistics: Who is Most Affected
Compulsive overeating is more common than it seems. Here are some key facts:
- Gender. Although the disorder occurs in both men and women, the latter are 1.5–2 times more likely to suffer from it. This is due to social pressure, the cult of thinness, and hormonal factors.
- Age. The peak incidence occurs between 18–35 years, but the first episodes may appear as early as adolescence. It is less common in children and the elderly.
- Social groups. The disorder is equally prevalent across income levels but is more common among those who:
- experience chronic stress (e.g., high-pressure jobs);
- have low self-esteem or a tendency toward depression;
- grew up in families where food was used as a reward or comfort.
Interestingly, about 40% of people with compulsive overeating have a normal weight, making diagnosis difficult. Many don’t even realize that their eating habits are not just a “weakness” but a medical issue requiring attention.
If you recognize yourself in this description—don’t despair. Compulsive overeating can be managed, and later in the article, we’ll explore how to cope with it.

Psychological Causes of Compulsive Overeating
Many mistakenly believe that compulsive overeating is simply a lack of willpower or a bad habit. In reality, its roots always lie in psychology. It is the psyche’s way of coping with things for which it has no other tools.
Why does this happen? Our brain seeks the simplest and fastest ways to obtain pleasure or relieve tension. Food is the most accessible of these. It genuinely helps—but only temporarily, creating a vicious cycle of dependency. To break it, you need to understand which psychological needs your body is trying to satisfy through overeating.
Emotional Triggers
- Stress, anxiety, boredom, loneliness. When we experience negative emotions, the brain urgently seeks a way to improve our state. Sweet and fatty foods trigger dopamine release—the pleasure hormone. This provides temporary relief, but the problem remains unresolved. Over time, a conditioned reflex forms: anxiety → food → temporary relief. As a result, a person starts eating not when hungry but when nervous, bored, or feeling lonely.
- Food as a way to cope with negative emotions. For many, food becomes a sort of “emotional crutch.” In childhood, we might have been comforted with sweets, and this behavioral pattern persists into adulthood. The problem is that this method of emotional regulation is ineffective in the long run – the emotions don’t disappear, and guilt over overeating is added to them.
Childhood Trauma and Conditioning
- Family eating habits (“finish your plate,” “food = love”). Many eating disorders stem from childhood. Beliefs like “your plate must be clean” or “you can’t waste food” force people to eat even when full. If food was used as an expression of love in the family (e.g., overfeeding with baked goods), an adult may subconsciously seek the same warmth and care through food.
- Using food as punishment or reward. When parents manipulate with food (“no dessert until you finish your homework” or “eat your soup, and you’ll get candy”), the child develops a distorted perception of eating. In adulthood, this can turn into a system of self-punishment and rewards using food, often leading to overeating.
Perfectionism and Self-Criticism
- The cycle of “breakdown → guilt → new breakdown.” This is especially pronounced in perfectionists. Even a slight deviation from “perfect” eating (e.g., having a slice of cake while dieting) triggers harsh self-criticism. The resulting guilt causes so much stress that the person “eases” it with another round of food—and the cycle repeats.
- Unattainable beauty standards and their influence. Social media and glossy magazines promote unrealistic beauty ideals. Constant comparison with these standards creates chronic stress, which many try to numb with food. At the same time, the act of overeating reinforces feelings of “falling short” of the ideal, creating a closed loop.
Lack of Pleasure in Life
If a person’s life lacks positive emotions, enjoyment, and engaging activities, food naturally becomes the main (and sometimes only) source of joy. This is especially common among people with limited social circles, unfulfilling jobs, or no hobbies. The brain simply sees no other way to get dopamine except through food.
Understanding these psychological mechanisms is the first step toward solving the problem. Once you recognize which needs you’re trying to satisfy through food, you can begin seeking healthier ways to fulfill them.

Practical Methods to Combat Compulsive Overeating
Compulsive overeating is a complex disorder, but it can and should be addressed. The good news: there are many effective methods to break the vicious cycle of “stress → overeating → guilt.” These approaches work on different levels—from changing daily habits to deep psychological work.
It’s important to understand that there is no magic pill for compulsive overeating. The process requires a comprehensive approach, but every small step brings you closer to freedom from food dependency. These methods are backed by research and real-life stories of people who have overcome the problem. Start with the ones that resonate most with you and gradually incorporate others.
Mindfulness and Self-Assessment
Food and Emotion Journaling
This tool is the foundation for addressing overeating. Record:
- What and when you ate.
- Hunger level on a scale of 1 to 10 before eating.
- Emotions and circumstances surrounding the meal.
- Feelings after eating.
Such a journal helps identify patterns: which emotions most often lead to overeating, what times of day trigger episodes, and which foods act as triggers. After 2-3 weeks of tracking, you’ll better understand your eating patterns.
The “5 Questions” Technique Before Eating
Before eating, ask yourself:
- Am I physically hungry right now?
- What emotions am I feeling?
- What am I trying to get from this food?
- How will I feel after eating this?
- Is there another way to meet this need?
These questions create a pause that often helps avoid impulsive overeating.
Alternative Ways to Cope with Stress
Exercise, Meditation, and Breathing Techniques
Physical activity is one of the healthiest ways to regulate emotions. Even a 10-minute walk can reduce stress levels. Meditation (especially mindfulness) and breathing exercises (e.g., the *”4-7-8″ method*) help calm the urge to “eat away” emotions in the moment.
Distracting Hobbies
Create a “menu of alternatives”—a list of activities to divert attention from food cravings:
- Drawing or stress-relief coloring books.
- Playing a musical instrument.
- Reading an engaging book.
- Handicrafts.
- Playing with a pet.
The key is to choose something that genuinely captivates you.
Normalizing Eating Habits
Avoiding Strict Diets
Rigid restrictions create a “forbidden fruit” effect—the more you deny yourself, the stronger the craving for “off-limits” foods. Instead of diets, transition to intuitive eating, a system where no foods are “bad,” but you pay attention to your body’s signals.
Balanced Nutrition to Reduce Binge Urges
Nutrient deficiencies often intensify cravings. Important steps:
- Include protein in every meal (it promotes fullness).
- Don’t eliminate healthy fats (they’re crucial for hormonal balance).
- Choose complex carbs (whole grains, vegetables).
- Don’t skip meals (this leads to overeating later).
Psychological Work
Cognitive Behavioral Therapy (CBT) for Compulsive Overeating
CBT is the gold standard for treating eating disorders. It helps:
- Identify and change automatic negative thoughts about food.
- Break the link between emotions and overeating.
- Develop new, healthy eating habits.
Self-Acceptance and Anxiety-Reduction Techniques
Practices like self-compassion and silencing your inner critic reduce the need to “eat away” stress. Try:
- The “kind friend” technique (how would you support a friend in this situation?).
- Body-positive affirmations.
- Grounding techniques for anxiety.
When to Seek Professional Help
Signs the Problem Is Out of Control
- Binge episodes more than once a week.
- Significant weight fluctuations.
- Depression or anxiety disorders.
- Failed attempts to manage it alone.
Who to Consult
- Clinical psychologist (specializing in eating disorders).
- Nutritionist (knowledgeable about compulsive overeating).
- Psychiatrist (if accompanied by depression or anxiety).
Remember: seeking professional help is not weakness – it’s a rational step toward recovery. Compulsive overeating is a complex disorder, and sometimes expert support is necessary to break the cycle.

Conclusion
Compulsive overeating is not about weak willpower or lack of self-control. It is a serious psychological disorder rooted in our emotions, childhood habits, and ways of coping with stress. It’s crucial to understand: you are not to blame for finding yourself in this trap. Guilt and shame only worsen the problem, creating a vicious cycle of “relapse → self-flagellation → new relapse.” But there’s good news—this cycle can be broken.
Don’t expect changes to happen overnight. Start small: try keeping a food journal, practice the “5 questions” technique before eating, find at least one new way to cope with stress without turning to food. Each of these steps is a building block in the foundation of your recovery. Remember: even small but consistent efforts lead to significant changes over time. Those who are free from compulsive overeating today also started with small steps.
Most importantly—don’t be afraid to ask for help. Seeking support from a psychologist, nutritionist, or support group is not a sign of weakness but an act of self-care. Many struggle alone for years, facing disappointment, when professional help could have accelerated the process. You have the right to assistance and support. Compulsive overeating is a solvable problem, and the sooner you take action, the sooner you’ll restore a healthy relationship with food and yourself.
You’ve already taken an important step—learning more about the issue. Now, it’s time to put this knowledge into practice. Trust the process, be patient with yourself—and change will come.