Schizophrenia is a serious mental disorder that affects a person’s thinking, perception, and behavior. This complex illness, surrounded by many myths and misconceptions, often causes fear and social rejection. However, understanding the facts about schizophrenia can help us better understand the condition and support those who live with it.
In this article, I will explore all aspects of schizophrenia in detail: from symptoms and causes to treatment methods and support strategies. The goal is to provide comprehensive information that will be useful to both patients and their loved ones, as well as anyone interested in understanding this disorder more fully.
What is Schizophrenia?
Schizophrenia is a chronic mental disorder characterized by disturbances in thinking, perception, and emotional responses. People with schizophrenia may experience hallucinations, delusional ideas, disorganized thinking and speech, as well as difficulties in communication, social interaction, and daily life.
It’s important to note that schizophrenia is not “split personality,” as is often mistakenly believed. It is a complex neurobiological disorder that affects various aspects of a person’s mental state.
Historical Background
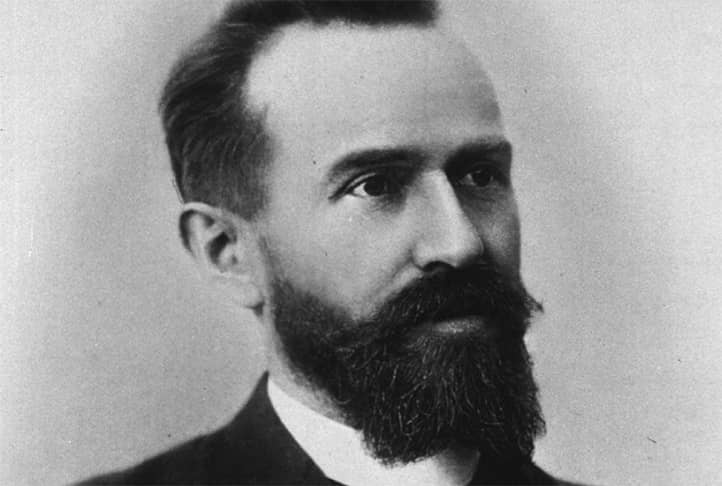
The term “schizophrenia” was introduced by the Swiss psychiatrist Eugen Bleuler in 1911. It derives from the Greek words “schizo” (split) and “phren” (mind), reflecting the idea of a split in mental functions associated with the condition.
However, the history of schizophrenia research began much earlier. In 1896, German psychiatrist Emil Kraepelin described a condition he called “dementia praecox” (early dementia), which was later recognized as an early description of schizophrenia.
Throughout the 20th century, our understanding of schizophrenia evolved significantly. From initial theories about “split personality” to modern neurobiological models, our comprehension of this disorder continues to develop.

Symptoms and Signs of Schizophrenia
Schizophrenia is a kaleidoscope of experiences, unique to each individual. Like an artist painting on the canvas of consciousness, this disorder creates vivid, often frightening images, sounds, and sensations that feel completely real to those who experience them.
Imagine looking at the world through a prism that distorts reality in the most unexpected ways. Ordinary objects may take on ominous meanings, and everyday sounds transform into mysterious messages. This is just part of what a person with schizophrenia might experience.
However, the symptoms of schizophrenia are not limited to vivid hallucinations and bizarre ideas. They may manifest in more subtle forms, unnoticed by others but profoundly affecting the individual’s inner world. Emotional detachment, loss of motivation, and difficulties in communication can be as disruptive as the more apparent symptoms of the illness.
Symptoms of schizophrenia are usually divided into three main categories: positive, negative, and cognitive. It’s important to understand that symptoms may vary significantly from person to person.
Positive Symptoms
Positive symptoms are those that “add” something to a person’s experience, which is not present in healthy individuals. These include:
- Hallucinations: false sensory perceptions. Auditory hallucinations (hearing voices) are most common, but visual, tactile, olfactory, or gustatory hallucinations can also occur.
- Delusional ideas: false beliefs that persist despite contradictory evidence. For example, a person may believe they are being watched or have supernatural powers.
- Disorganized thinking and speech: difficulties in logical thinking and expressing thoughts. Speech may be incoherent or inconsistent.
- Behavioral disturbances: from agitated, unpredictable behavior to catatonia (a state of immobility).
Negative Symptoms
Negative symptoms are associated with a “loss” or reduction in normal functions. They include:
- Emotional flatness: reduced expression of emotions through facial expressions, voice tone, or gestures.
- Anhedonia: inability to experience pleasure from activities that usually bring joy.
- Avolition: lack of motivation or initiative.
- Social isolation: reduced social contact and interaction.
- Alogia: decreased speech activity or content.
Cognitive Symptoms
Cognitive symptoms affect mental abilities:
- Attention and concentration difficulties.
- Working memory problems.
- Difficulty in planning and organizing activities.
- Slowed information processing.
These symptoms can greatly impact the daily life and functioning of a person with schizophrenia, making work, studies, and social interactions challenging.

Causes and Risk Factors of Schizophrenia
Schizophrenia is a mystery that scientists have been trying to solve for decades. Like a detective gathering clues, researchers collect information piece by piece about possible causes of this complex disorder.
Imagine the brain as an incredibly complex computer where billions of neurons form an unimaginably intricate network. Schizophrenia may arise when failures occur in this network, much like how a small error in code can lead to unpredictable behavior across the entire system.
However, the brain does not exist in a vacuum. It constantly interacts with its environment, responding to stresses, trauma, and even subtle changes in our body’s chemistry. This intricate “ecosystem” creates unique conditions in which schizophrenia may develop.
The exact causes of schizophrenia remain poorly understood, but studies indicate a complex interaction of genetic, environmental, and neurobiological factors.
Genetic Factors
Genetics play a significant role in the development of schizophrenia:
- Hereditary: People with close relatives who have schizophrenia have a higher risk of developing the disorder. If one of the identical twins has schizophrenia, the likelihood that the other twin will develop it is about 50%.
- Genetic variations: Studies have identified numerous genes that may increase the risk of schizophrenia. However, there is no single “schizophrenia gene” — rather, it’s a complex interaction of many genetic variations.
- Epigenetics: Environmental factors can affect gene expression, which may also play a role in the development of schizophrenia.
Environmental Factors
Various environmental factors can increase the risk of developing schizophrenia:
- Prenatal factors: Complications during pregnancy and childbirth, such as infections, malnutrition, or maternal stress, can increase the risk.
- Childhood trauma: Psychological trauma, abuse, or neglect in childhood is associated with an increased risk of developing schizophrenia.
- Substance use: Abuse of certain drugs, especially cannabis during adolescence, can increase the risk of psychosis.
- Socioeconomic factors: Urbanization, migration, and low socioeconomic status are also associated with an increased risk of schizophrenia.
Neurobiological Aspects
Research has also identified several neurobiological features:
- Structural changes: People with schizophrenia often show changes in gray matter volume and ventricle size in the brain.
- Neurochemical imbalance: Disturbances in neurotransmitter systems, particularly dopamine and glutamate, play a crucial role in the pathophysiology of schizophrenia.
- Neuronal connectivity: Studies show disruptions in the functional connectivity of various brain regions in people with schizophrenia.
- Neuroinflammation: Some studies point to the role of inflammatory processes in the brain in the development of schizophrenia.
It’s important to note that schizophrenia likely results from a complex interaction of all these factors, rather than any single cause.

Diagnosis of Schizophrenia
Diagnosing schizophrenia is an art that requires not only deep knowledge but also refined intuition. Like an experienced wine taster who can detect various flavors in a glass of wine, an experienced psychiatrist can pick up on subtle nuances in a patient’s behavior and speech that may indicate the presence of schizophrenia.
However, unlike many physical illnesses, schizophrenia cannot be diagnosed with a simple blood test or X-ray. This disorder manifests in the very essence of what makes us human — our thoughts, emotions, and perception of the world.
The process of diagnosing schizophrenia is akin to assembling a complex mosaic. Each symptom, each detail of the patient’s history is a separate piece that needs to be arranged correctly to see the full picture. And sometimes, it takes time and patience for this picture to emerge.
Diagnosing schizophrenia is a complex process that requires thorough clinical assessment and observation. There is no single test that can definitively diagnose this disorder.
Diagnostic Criteria
Schizophrenia is diagnosed based on criteria described in diagnostic manuals such as the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) or the ICD-11 (International Classification of Diseases).
According to DSM-5, at least two of the following symptoms must be present for a significant portion of time during a one-month period (or less if successfully treated) to diagnose schizophrenia:
- Delusional ideas
- Hallucinations
- Disorganized speech
- Grossly disorganized or catatonic behavior
- Negative symptoms
Additionally, there should be a decline in functioning in one or more major areas of life (work, interpersonal relationships, self-care), and symptoms must persist for at least six months.
Examination Methods
The diagnostic process usually includes the following steps:
- Clinical interview: A detailed conversation with the patient about their symptoms, medical history, and life circumstances.
- Physical examination: To rule out other medical conditions that may cause similar symptoms.
- Psychological testing: May include tests for cognitive functions, personality traits, and severity of symptoms.
- Laboratory tests: To rule out other medical causes of symptoms (e.g., endocrine disorders or drug use).
- Neuroimaging: MRI or CT scans of the brain may be ordered to rule out structural brain abnormalities.
- Observation: A period of observation is often required to confirm the diagnosis and assess symptom dynamics.
It is important to note that the diagnosis of schizophrenia requires ruling out other mental disorders, such as bipolar disorder or clinical depression with psychotic features, as well as ruling out the direct physiological effects of substance use or other medical conditions.
Early diagnosis and intervention are crucial for improving the long-term prognosis of schizophrenia. However, due to the complexity and variability of symptoms, as well as the stigma associated with mental illness, many people with schizophrenia do not receive prompt diagnosis and treatment.

Treatment of Schizophrenia
Treating schizophrenia is akin to a journey through uncharted territory. Doctors and patients together create a map for this journey, marking hazardous areas, finding safe routes, and discovering new horizons. Every step forward is a victory, every obstacle an opportunity to learn something new.
Modern psychiatry offers a wide array of tools to treat schizophrenia. From the latest antipsychotic medications to innovative psychotherapy methods, this is like a set of keys, each one capable of opening a door to a better life. The physician’s task is to find the keys that fit each patient’s unique needs.
Treatment of schizophrenia generally involves a comprehensive approach, combining medication, psychotherapy, and social support. The goal of treatment is to reduce symptoms, improve quality of life, and help the individual adapt within society.
Medication
Medication forms the foundation of schizophrenia treatment, with antipsychotic drugs helping to control symptoms, particularly positive ones such as hallucinations and delusional thinking.
- Typical Antipsychotics (first-generation): These drugs, such as haloperidol, were the first effective treatments for schizophrenia. They are effective in controlling positive symptoms but can cause significant side effects, including extrapyramidal symptoms.
- Atypical Antipsychotics (second-generation): These newer drugs, like risperidone, olanzapine, and quetiapine, generally cause fewer side effects and may be more effective for treating negative symptoms.
- Other Medications: Depending on symptoms and comorbid conditions, antidepressants, mood stabilizers, or anxiolytics may be prescribed.
It’s important to note that finding the right medication and dosage often takes time and requires close collaboration between the patient and physician.
Psychotherapy
Psychotherapy plays a significant role in the comprehensive treatment of schizophrenia:
- Cognitive Behavioral Therapy (CBT) helps patients recognize and change maladaptive thoughts and behaviors. CBT is especially beneficial for managing positive symptoms and reducing the risk of relapse.
- Family Therapy involves the patient’s family in the treatment process, teaching them supportive strategies and improving communication.
- Social Skills Training assists patients in developing communication and problem-solving skills, which can improve their social adaptation.
- Psychoeducation provides patients and their families with information about the illness, its symptoms, and treatment methods, enhancing treatment adherence and symptom management.
- Supportive Psychotherapy offers emotional support and helps patients cope with daily challenges.
Social Support
Social support plays a crucial role in treating schizophrenia:
- Vocational Rehabilitation assists patients in finding and maintaining jobs, which improves their financial independence and self-esteem.
- Support Groups allow patients to interact with others who have similar experiences, share coping strategies, and receive emotional support.
- Service Coordination and Healthcare Navigation: Ensures patients receive all necessary services, including healthcare and social support.
- Organization of Social and Recreational Activities: Helps patients remain active and socially engaged.
It’s important to understand that treating schizophrenia is a long-term process, and often a combination of different approaches is necessary for the best results. An individualized treatment plan should consider each patient’s unique needs and circumstances.

Living with Schizophrenia
Living with schizophrenia is like being an actor in a play where the script is constantly changing. Each day can bring new challenges and unexpected plot twists, demanding flexibility and adaptation.
Imagine trying to complete a puzzle where some pieces continually change shape or disappear. This can resemble the experience of someone with schizophrenia attempting to organize daily life. Simple tasks may become complex, while familiar things seem unfamiliar.
However, life with schizophrenia is not solely about struggle and hardship. Many people with this diagnosis find incredible strength and creativity within themselves. They learn not only to live with their condition but to use their unique experience to create art, develop empathy, and gain a deeper understanding of human nature.
Everyday Challenges
People with schizophrenia may face various challenges in daily life:
- Cognitive Difficulties: Problems with concentration, memory, and organization can make daily tasks and work more challenging.
- Social Isolation: Negative symptoms and stigma often lead to reduced social contact.
- Employment Difficulties: Symptoms of the illness and medication side effects may complicate finding and maintaining a job.
- Self-Care Challenges: Some patients struggle with self-care tasks, including hygiene and meal preparation.
- Financial Issues: Difficulty finding work and treatment costs often lead to financial hardships.
- Medication Side Effects: Antipsychotic medications can cause a range of side effects that impact daily life.
Coping Strategies
Several strategies can help people with schizophrenia manage everyday challenges more effectively:
- Adherence to Treatment: Regularly taking medication and attending therapy is essential for controlling symptoms.
- Establishing and Following a Routine: A structured daily routine helps manage symptoms and daily tasks.
- Healthy Lifestyle: Regular exercise, a balanced diet, and sufficient sleep improve overall well-being and symptom management.
- Relaxation Techniques: Practices such as meditation or diaphragmatic breathing help reduce stress and anxiety.
- Social Support: Maintaining connections with family and friends and participating in support groups helps overcome social isolation.
- Cognitive Strategies: Using reminders, lists, and other organizational tools helps manage cognitive difficulties.
- Self-Education: Learning about the illness allows patients to better understand their condition and manage symptoms.
- Developing Coping Skills: Working with a therapist to develop specific skills for managing symptoms and stress.

Myths and Misconceptions about Schizophrenia
Schizophrenia is shrouded in myths and misconceptions, like an ancient castle surrounded by legends. These myths, passed down through the years, often distort the true nature of the illness, creating barriers between people with schizophrenia and society.
Imagine looking at the world through a distorted mirror. Everything appears skewed and does not reflect reality. Similarly, myths about schizophrenia distort the truth, creating false and often frightening images.
Dispelling these myths requires effort and patience, but it is essential to pave the way for understanding and acceptance of people with schizophrenia in society.
- Myth – People with schizophrenia have split personalities.
Fact: Schizophrenia and dissociative identity disorder are different conditions. Schizophrenia does not involve “multiple personalities.”
- Myth – All people with schizophrenia are dangerous and prone to violence.
Fact: Most people with schizophrenia are not dangerous. In fact, they are more likely to be victims of violence than its perpetrators.
- Myth – Schizophrenia is a result of poor upbringing or weak willpower.
Fact: Schizophrenia is a biological brain disorder caused by a complex interplay of genetic and environmental factors.
- Myth – Schizophrenia cannot be cured; it’s a lifelong sentence.
Fact: While a complete cure for schizophrenia is not yet available, many people with this condition respond well to treatment and can lead fulfilling lives.
- Myth – People with schizophrenia cannot work or study.
Fact: With proper treatment and support, many people with schizophrenia successfully work, study, and lead active social lives.
- Myth – Schizophrenia is a rare condition.
Fact: Schizophrenia affects about 1% of the global population, making it a relatively common disorder.
- Myth – Schizophrenia always appears in adolescence or early adulthood.
Fact: Although this is the most common age for the onset of schizophrenia, it can develop at any age.
Dispelling these myths and spreading accurate information about schizophrenia helps reduce stigma and fosters better understanding and support for people with the condition.

Support for Patients and Their Families
Support for people with schizophrenia and their families is like a lifebuoy in stormy seas. It provides the strength to stay afloat when the waves seem insurmountable, guiding the way to a shore of hope and recovery.
Imagine a network woven from threads of empathy, knowledge, and practical help. This network can keep a person from falling into the abyss of isolation and despair, offering them a foundation to move forward.
Support is not merely words of comfort or financial aid. It is a whole ecosystem of resources, including professional assistance, support groups, educational programs, and much more. Each element of this system plays a role in creating an environment where a person with schizophrenia can not only survive but thrive.
Support Groups
Support groups provide invaluable assistance:
- For Patients: Support groups for people with schizophrenia offer the opportunity to share experiences, coping strategies, and emotional support.
- For Families: Support groups for relatives help manage stress, share information, and exchange caregiving strategies for a loved one with schizophrenia.
- Online Communities: Internet forums and social media groups can provide support and information, especially for those unable to attend in-person meetings.
Resources and Organizations
Many organizations and resources offer information and support:
- National Mental Health Associations: In many countries, national organizations provide information, advocacy, and support.
- Local Clinics and Hospitals: Often offer support programs and educational resources for patients and families.
- Educational Programs: Many organizations provide courses and seminars to educate patients and their families about schizophrenia and coping strategies.
- Helplines: Provide immediate support in crisis situations.
- Advocacy Organizations: Work to improve the rights and living conditions of people with mental health disorders.
- Vocational Rehabilitation Programs: Help people with schizophrenia find and retain employment.
- Housing Programs: Provide support in securing appropriate housing.
It is important to note that the availability of specific resources and organizations may vary depending on the country and region. Local healthcare services or mental health organizations can be a valuable source of information on available resources.
Conclusion
Schizophrenia is a complex mental disorder that challenges not only those who live with it but also society as a whole. It affects the deepest aspects of human experience – our perception of reality, thoughts, and emotions. Despite the complexity of this condition, modern science and medicine offer hope and pathways for improving the quality of life for people with schizophrenia.
The key to effectively managing schizophrenia lies in a comprehensive approach that combines medication, psychotherapy, and social support. It is crucial to remember that each case of schizophrenia is unique, and treatment should be individualized to meet the specific needs and circumstances of each person.
Fighting stigma and spreading accurate information about schizophrenia play a vital role in enhancing the lives of people with this condition. The more society understands the nature of schizophrenia, the easier it will be to create an environment where individuals with this diagnosis can lead full lives, realize their potential, and contribute to society.
Research in the field of schizophrenia continues to unveil new horizons. From genetic studies to innovative treatment methods, our understanding of this complex disorder is deepening continuously. These advancements provide hope for the development of more effective treatments and perhaps even the prevention of schizophrenia in the future.