Clinical depression is a serious mental illness characterized by persistent sadness, loss of interest in life, and a lack of pleasure in usual activities, which significantly affects a person’s daily life. It goes beyond normal mood fluctuations and short-term emotional reactions to current life challenges.
Clinical depression, also known as major depressive disorder, is accompanied by a wide range of symptoms, including significant loss of energy, changes in appetite and sleep, difficulties concentrating, feelings of hopelessness and helplessness, as well as thoughts of death or suicide. For this condition to be diagnosed, symptoms must be present almost every day for at least two weeks.
Treatment of clinical depression typically involves a combination of psychotherapy and medication. The approach to treatment is individualized and may take time to find the most effective combination of methods. It is important to note that with timely and adequate treatment, most people with clinical depression experience significant improvement in their condition.
The topic of clinical depression deserves attention due to its widespread prevalence and serious impact on people’s lives. Clinical depression can significantly deteriorate the quality of life, affect personal and professional relationships, and impair the ability to perform daily tasks. Moreover, this condition is associated with an increased risk of developing chronic diseases and can lead to suicidal thoughts and attempts.
Discussing and highlighting this topic helps to break the stigma and myths surrounding mental illness and emphasizes the importance of seeking timely help and support. The importance of the topic also lies in the need to inform the public about the symptoms, methods of diagnosis, and available treatment options, which can contribute to early detection and effective management of the condition.
The understanding of clinical depression has evolved significantly throughout history, from ancient times to the present, reflecting changes in societal views on mental health and advancements in medicine.
In ancient times, clinical depression was often viewed as a manifestation of evil spirits or divine punishment. In Greco-Roman medicine, Hippocrates described a condition resembling depression as “melancholy,” which he associated with an imbalance of bodily fluids. In the Middle Ages, depression could be seen as a spiritual trial or witchcraft.
During the Renaissance, a shift toward a more humanistic view of mental disorders began. Philosophers and doctors of the Enlightenment period started emphasizing the role of the mind and emotions in mental disorders, moving away from supernatural explanations.
In the 19th century, with the formation of psychiatry as a science, the systematic study of depression began. Emil Kraepelin and other pioneers of psychiatry differentiated various forms of mental illness, including depression, as a distinct condition.
The 20th century saw significant progress in understanding and treating depression. The discovery of antidepressants in the mid-century revolutionized treatment approaches. Psychoanalytic and behavioral theories offered various explanations for the mechanisms of depression and methods of therapy.
With the development of neuroscience and genetics in the 21st century, the biological underpinnings of depression became better understood. There has been a deepening understanding of the role of neurotransmitters, genetic predisposition, and environmental influences on the development of depression. The emergence of cognitive-behavioral therapy and other forms of psychotherapy has enriched the range of treatment methods.
Today, clinical depression is recognized as a complex disorder requiring a comprehensive approach that integrates medical, psychological, and social aspects. Research continues to further understand this condition and develop more effective treatment methods.

Causes of Clinical Depression
Clinical depression is a complex condition arising from a combination of diverse factors. The scientific community agrees that there is no single cause that can lead to clinical depression. A mosaic of biological, psychological, and social elements contributes to its development, making each case of the disorder unique.
Biological aspects include genetic predisposition and changes in brain chemistry. This further emphasizes that our physiology can influence mental health. Psychological factors reveal how our thoughts, feelings, and ways of coping with stress can contribute to the development of depressive states. At the same time, social and environmental causes, such as relationships, work environment, and life circumstances, play an equally significant role, highlighting how the external world interacts with our inner state.
Understanding how these various elements intersect and influence one another is vital for developing effective strategies for treating and supporting individuals with clinical depression. By opening the door to a deep understanding of the causes of this condition, we are moving closer to understanding its essence and the best ways to help those who need it.
Biological Factors
Biological factors contributing to the development of clinical depression represent a complex network of interactions between genetic, neurochemical, and physiological aspects of the human body. These factors highlight how innate and biochemical elements can lead to depressive disorders.
- Genetic predisposition plays a significant role, indicating that the likelihood of developing depression may be higher in individuals with a family history of the disorder. Twin and family studies show that if one identical twin has clinical depression, the likelihood of the other twin developing it is significantly higher than in the general population.
- Neurochemical factors also play a critical role. An imbalance of certain chemicals in the brain, such as serotonin, norepinephrine, and dopamine, which regulate mood and emotions, can lead to depression symptoms. Medication aimed at correcting this imbalance is often effective in improving symptoms.
- Physiological changes and illnesses can also increase the risk of developing depression. For example, thyroid diseases, cardiovascular conditions, and certain hormonal disorders can affect mood and overall well-being, contributing to depressive states.
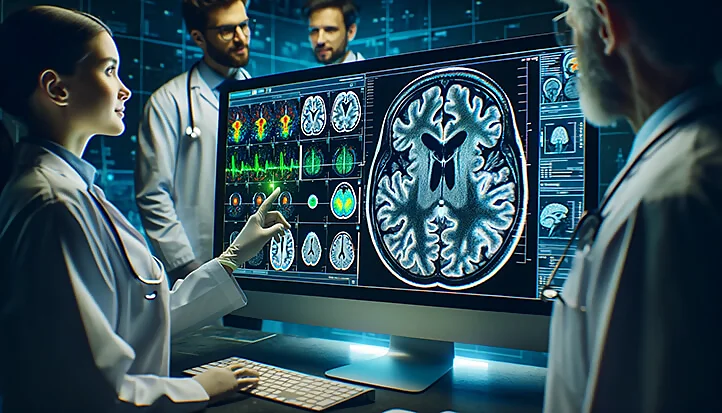
- Structural changes in the brain, such as a reduction in the volume of certain areas responsible for mood regulation, have been observed in some individuals with clinical depression. These changes may be related to both genetic factors and the impact of stress and other external circumstances.
Overall, biological factors highlight the complexity and multifaceted nature of the origins of clinical depression, confirming the need for a comprehensive approach to diagnosing and treating this condition.
Psychological Factors
Psychological factors influencing the development of clinical depression reflect the internal world of the individual, including their thoughts, feelings, and experiences. These factors can include personality traits, coping mechanisms, and reactions to life events.
- Personality traits may increase vulnerability to depression. Such traits include low self-esteem, pessimism, perfectionism, and a tendency toward self-criticism. People with these characteristics experience failures and stressful situations more acutely, which increases the risk of developing depressive disorders.
- Information processing and cognitive distortions also play a significant role. For example, a tendency toward negative thinking, catastrophizing, and generalizing negative experiences can exacerbate feelings of hopelessness and loss of control, leading to depression. Cognitive-behavioral therapy often targets the correction of these distorted beliefs.
- Coping strategies for stress significantly impact an individual’s psychological resilience. Maladaptive coping mechanisms, such as avoiding problems, suppressing emotions, or abusing alcohol, can contribute to the development of depression. In contrast, developing adaptive coping skills, such as problem-solving, seeking social support, and relaxation, can serve as protective factors.
- Traumatic events and stress often precede the onset of depression. These may include both single events, such as the loss of a loved one or a severe injury, and prolonged stressful circumstances, including chronic family or workplace conflicts, prolonged financial hardship, or health problems.
- Self-perception and worldview also affect psychological well-being. Feelings of hopelessness, an inability to control one’s life, and a lack of purpose can worsen depression, creating a vicious cycle of negative self-perception and emotional decline.
Addressing psychological factors requires a comprehensive approach, including psychotherapy, stress management training, and, if necessary, pharmacotherapy. Understanding and working through psychological aspects can significantly aid in recovery and prevent depression relapse.
Socioeconomic Factors
Socioeconomic factors play an important role in the development and course of clinical depression, reflecting the influence of the external environment and societal conditions on an individual’s mental health. These factors can include economic status, social support, living and working conditions, as well as cultural and societal norms.
- Economic status significantly influences the risk of developing depression. Low income, poverty, and financial instability often lead to increased stress, feelings of hopelessness, and isolation. The struggle for survival and lack of resources to meet basic needs can exacerbate feelings of despair and hopelessness.
- Social support is a key factor in preventing and treating clinical depression. Having strong, supportive relationships with family, friends, and the community can serve as a buffer against mental disorders. Loneliness and social isolation, on the other hand, increase vulnerability to depression.
- Working conditions and employment also impact mental health. High levels of work-related stress, job insecurity, exhausting or underpaid work can contribute to the development of depressive states. A balance between work and personal life, as well as job satisfaction, is essential for mental well-being.
- Education and access to information about mental health play a significant role in awareness and seeking help for clinical depression. A higher level of education and access to quality information can promote earlier medical intervention and effective treatment.
- Cultural and societal norms also influence the perception and stigmatization of depression. In some cultures, discussing mental health issues is taboo, which prevents people from seeking help.
In general, socioeconomic factors emphasize the need for a comprehensive approach to preventing and treating clinical depression, including improving living conditions, increasing the availability and quality of medical and social services, and promoting social support and inclusion.

Symptoms of Clinical Depression
Clinical depression manifests through a variety of symptoms affecting both the physical and mental state of a person. These symptoms can vary significantly between individuals, reflecting the uniqueness of each case. Recognizing these symptoms is a key step towards diagnosis and subsequent treatment. It is important to understand that depression is not limited to just feelings of sadness or melancholy; it can affect a person’s ability to function, their work, relationships, and overall well-being.
The diagnosis of clinical depression requires a thorough analysis of the symptoms, their duration, and their impact on a person’s life. Specialists use established clinical criteria to determine the presence and severity of depressive disorders. The diagnostic process may involve both discussions with the patient and the use of specialized diagnostic tools and questionnaires.
Understanding the symptoms and methods of diagnosis is crucial not only for medical professionals but also for the general public. Awareness of the signs of depression enables individuals and their loved ones to seek help in a timely manner and contributes to reducing the stigma associated with seeking psychological support.
Main Symptoms
The main symptoms of clinical depression can vary in intensity and manifestation, but overall they cover a broad range of emotional, physical, and cognitive aspects that affect a person’s daily life. Here are the most common signs and symptoms:
- Persistent feelings of sadness or emptiness. Patients often describe a feeling of a “black hole” inside or an inability to experience joy from activities that used to bring pleasure.
- Loss of interest in usual activities. A decrease in interest or pleasure from hobbies, social activities, or work, known as anhedonia.
- Significant changes in appetite and weight. This can involve either a loss of appetite and weight loss or an increased appetite and weight gain.
- Sleep disturbances. Insomnia or, conversely, an excessive desire to sleep (hypersomnia) may be signs of depression.
- Increased fatigue or loss of energy. A constant feeling of tiredness even without significant physical exertion, a decrease in energy and motivation.
- Restlessness, nervousness, or irritability that was not previously characteristic.
- Feelings of worthlessness or excessive guilt. Painful feelings of personal inadequacy or a sense of unwarranted guilt over past events.
- Decreased thinking ability and concentration. Problems with focusing attention, memory, or decision-making.
- Recurrent thoughts of death, suicide, or suicide attempts.
These symptoms significantly hinder the ability to carry out daily responsibilities and impact interpersonal relationships, work, and overall quality of life. It is important to note that the presence of several of these symptoms, especially if they persist for two weeks or more, may indicate the need to seek professional help.
Diagnostic Criteria
The diagnostic criteria for clinical depression are outlined in standard classifications such as the Diagnostic and Statistical Manual of Mental Disorders (DSM) by the American Psychiatric Association and the International Classification of Diseases (ICD) by the World Health Organization. These criteria help doctors and therapists determine the presence and severity of major depressive disorder (MDD) in patients. Below is a summary of the criteria based on the latest edition of the DSM (DSM-5):
- Presence of five or more of the following symptoms during a two-week period, with at least one of the symptoms being either depressed mood or loss of interest or pleasure:
- Almost daily depressed mood most of the day.
- Significant loss of interest or pleasure in all or almost all activities nearly every day.
- Significant weight change (weight loss or gain) without dieting or a change in appetite.
- Insomnia or excessive sleep almost every day.
- Psychomotor agitation or retardation almost every day.
- Fatigue or loss of energy almost every day.
- Feelings of worthlessness or excessive guilt nearly every day.
- Diminished ability to think or concentrate, or indecisiveness nearly every day.
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, suicide attempts, or a specific plan for committing suicide.
- The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- The symptoms are not due to the physiological effects of a substance (e.g., a drug, medication) or another medical condition (e.g., hypothyroidism).
- The condition is not better explained by other mental disorders (e.g., schizoaffective disorder, schizophrenia).
- The individual has never experienced manic or hypomanic episodes.
These criteria emphasize the need for thorough clinical evaluation in diagnosing clinical depression. It is important that diagnosis and treatment are conducted by qualified professionals capable of considering the complexity and multifaceted nature of the condition.
Differences Between Clinical Depression and Temporary Sadness
Clinical depression and temporary sadness are two different conditions, although they may have similar symptoms. It is important to understand their differences in order to properly approach treatment and support for individuals suffering from these conditions.
Clinical Depression
Clinical depression, also known as major depressive disorder, is a serious medical condition that affects many aspects of a person’s life. It is characterized by long-lasting and persistent feelings of sadness, hopelessness, and loss of interest in everyday life. The symptoms of clinical depression include significant changes in appetite and weight, sleep disturbances, fatigue, feelings of worthlessness or guilt, difficulties in concentration, and thoughts of death or suicide. These symptoms last for at least two weeks and cause significant difficulties in daily life.
Temporary Sadness
Temporary sadness or a bad mood is a normal part of human emotions that may arise in response to specific events or circumstances, such as stress at work, family problems, or personal loss. Usually, this condition passes on its own over a short period of time once the cause of the sadness is resolved. People experiencing temporary sadness may feel down and apathetic, but these feelings are usually not intense or long-lasting enough to seriously affect their everyday lives.
Key Differences
- Duration and intensity. Clinical depression is characterized by long-lasting, intense feelings of sadness and apathy, while temporary sadness is usually short-lived and less intense.
- Impact on daily life. Clinical depression significantly affects a person’s ability to function, including work, studies, relationships, and interest in activities. Temporary sadness does not have such profound consequences.
- Need for treatment. Clinical depression requires professional treatment, including psychotherapy, medication, or a combination of both. Temporary sadness usually resolves on its own or can be alleviated by self-help methods such as rest, physical exercise, or socializing with friends.

Treatment of Clinical Depression
In the fight against clinical depression, it is important to remember that this condition is treatable, and many people find a path to significant improvement in their well-being and return to a fulfilling life. Modern medicine and psychotherapy offer a wide range of treatment methods capable of alleviating depression symptoms and aiding in recovery. The approach to each person’s treatment is individualized and may include a combination of various strategies tailored to their unique needs and circumstances.
The journey to recovery begins with acknowledging the problem and seeking professional help. This can be a difficult step, especially given the stigma that still exists around mental illness. However, the decision to seek help is a key moment that opens the door to treatment and improving quality of life.
Treating depression is a process that requires time, patience, and collaboration between the patient and healthcare professionals. It may include medication to correct chemical imbalances in the brain, various forms of psychotherapy to address the cognitive and emotional aspects of the disorder, as well as lifestyle changes to support physical and mental health.
It is important to remember that the treatment of depression is not just about relieving symptoms but also about understanding and resolving underlying issues that contribute to the development of the disorder, as well as learning strategies to cope with life challenges more effectively and prevent future relapses.
Medication Treatment
Medication treatment of clinical depression is one of the key components of a comprehensive approach to therapy for this condition. It is aimed at correcting the chemical imbalance in the brain, which is considered one of the main causes of depressive disorders. The variety of available antidepressants allows for individualized treatment tailored to the patient’s specific symptoms, medical history, and response to previous treatments.
Antidepressants
Antidepressants are a class of medications designed to treat depression by acting on the brain’s neurotransmitter system, including serotonin, norepinephrine, and dopamine. There are several main types of antidepressants:
- Selective serotonin reuptake inhibitors (SSRIs). They increase serotonin levels in the brain, helping to improve mood and emotional state.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). These medications increase levels of both serotonin and norepinephrine, offering another mechanism to enhance mood.
- Tricyclic antidepressants (TCAs). An older class of drugs that may be used when newer antidepressants are ineffective.
- Monoamine oxidase inhibitors (MAOIs). One of the earliest types of antidepressants, used to treat certain types of depression when other medications are not helpful.
In some cases, additional medications may be prescribed to enhance the effect of antidepressants or to treat accompanying symptoms such as anxiety, insomnia, or obsessive thoughts.
The choice of a specific antidepressant and its dosage depends on many factors, including the severity of depression symptoms, previous responses to treatment, interactions with other medications, and potential side effects. It is important to work closely with a doctor to find the most suitable medication and dosage, and to regularly discuss treatment effectiveness and any side effects.
Medication treatment of clinical depression does not work immediately. It may take some time before the patient feels an improvement in their condition. In most cases, mood improvement begins a few weeks after starting the medication. Therefore, to prevent relapse, it is important to continue taking the medications for the recommended period, even if symptoms have improved.
Psychotherapy
Psychotherapy is a fundamental element in the treatment of clinical depression, providing a space to understand and resolve underlying causes, as well as to develop strategies for coping with symptoms and preventing relapses. This approach to treatment involves communication with a qualified psychologist or psychotherapist and can take many forms, depending on the individual’s needs and specific circumstances of their illness.
Types of Psychotherapy for Treating Depression
- Cognitive-behavioral therapy (CBT) focuses on identifying and changing negative thoughts and behavioral patterns that contribute to depression. CBT helps develop problem-solving skills and applies relaxation techniques to reduce stress.
- Psychodynamic therapy involves exploring past experiences and unconscious thoughts to understand how they affect current behavior and emotional state. The goal is to resolve internal conflicts that contribute to depression.
- Interpersonal therapy (IPT) focuses on improving interpersonal relationships and communication skills. IPT helps address social factors that contribute to the development and maintenance of depression, such as relationship conflicts or adaptation to life changes.
- Group therapy provides the opportunity to discuss problems in a group of people with similar difficulties under the guidance of a therapist, allowing participants to feel support, understanding, and relief.
Benefits of Psychotherapy
- Individualized approach. Psychotherapy is tailored to the individual needs and goals of each patient, making it effective for most people.
- Skills. It teaches long-term strategies for coping with stress, negative thoughts, and emotional difficulties, helping to prevent future episodes of depression.
- Deep understanding. Psychotherapy helps patients better understand the roots of their emotional problems and develop healthier ways of interacting with themselves and the world around them.
Psychotherapy can be conducted alone or in combination with medication. The decision on which treatment methods to use should be made by the doctor in collaboration with the patient, considering the specifics of the illness and the patient’s preferences.

The Impact of Clinical Depression on Daily Life
Clinical depression is not just a bad mood or sadness that disappears on its own. It is a serious medical condition that profoundly affects all aspects of a person’s life, from their internal world to their interactions with others. The intensity of this illness can change a person’s self-perception, their understanding of their place in the world, and their ability to find pleasure and meaning in everyday life.
Understanding the depth and variety of ways in which clinical depression can affect a person’s life is essential for an effective approach to treatment and support. The illness leaves its mark on physical health, emotional well-being, social relationships, and professional activities, requiring a comprehensive and multifaceted approach to recovery.
Clinical depression can manifest differently in each person, reflecting the uniqueness of their experience and circumstances. Recognizing this fact is crucial not only in choosing treatment methods but also in understanding what changes are necessary to alleviate symptoms and restore quality of life.
Impact on Personal Life
Clinical depression deeply affects a person’s personal life, influencing their relationships with loved ones, self-perception, and ability to enjoy life. The impact on personal life is multifaceted and can manifest in various forms.
- Relationships with loved ones. Depression creates tension in relationships with family, friends, and partners. The person may withdraw, become less communicative, and avoid social interactions, leading to increased feelings of loneliness and isolation for both themselves and their loved ones. Constant feelings of fatigue and apathy interfere with participation in family activities or social life, diminishing the sense of connection and belonging.
- Self-perception and self-esteem. Clinical depression is often accompanied by negative self-perception and low self-esteem. The person may feel worthless, guilty, or ashamed, deepening the depression and creating a vicious cycle of negative thinking. These feelings can make it difficult to accept oneself and one’s achievements, affecting personal growth and development.
- Interests and hobbies. Depression reduces interest in hobbies and activities that previously brought pleasure. The loss of enjoyment from activities like art, sports, or reading diminishes quality of life and limits opportunities for relaxation and self-expression.
- Sexual life. Clinical depression negatively affects sexual life, decreasing libido and interest in sexual activity. This can create additional tension in romantic relationships and reduce feelings of closeness with a partner.
- Ability to care for oneself. A person suffering from depression may struggle with completing daily self-care tasks, including hygiene, nutrition, and health management. This not only affects physical well-being but also reinforces dissatisfaction with oneself and worsens overall well-being.
Overcoming the impact of depression on personal life requires time, patience, and support from professionals and loved ones. It is important to recognize that depression is not a life sentence, and there are effective treatments that can help restore joy in life and improve the quality of personal relationships.
Impact on Work and Studies
Clinical depression significantly affects work and studies, influencing productivity, concentration, and overall engagement in professional and academic activities. These changes not only interfere with current responsibilities but can also have long-term consequences for career and educational prospects.
- Productivity and concentration. Depression can drastically reduce the ability to concentrate and focus on tasks. This leads to increased time spent completing work, decreased quality of results, and missed deadlines. In an academic setting, students may struggle to absorb new material, prepare for exams, and complete coursework.
- Attendance at work and school. Physical symptoms of depression, such as fatigue and sleep problems, can lead to frequent tardiness or absenteeism. This, in turn, can affect colleagues’ and teachers’ perceptions and reduce opportunities for career advancement or successful completion of academic courses.
- Interaction with colleagues and classmates. Depression can make communication and collaboration with colleagues and classmates difficult. Feelings of isolation or misunderstanding from others intensify social withdrawal, further reducing motivation and interest in work or studies.
- Decision-making and creativity. A decreased ability to engage in critical thinking and decision-making is another consequence of depression, which can hinder the successful resolution of work tasks or academic challenges. Creativity also declines, which is especially critical in professions requiring innovative approaches and creative thinking.
- Career development. The long-term impact of depression on work and studies can limit professional growth and career advancement. Problems with task completion, lack of initiative, and low overall productivity often result in missed opportunities for promotion or career development.
Impact on Physical Health
Clinical depression not only affects a person’s mental state but can also have serious consequences for their physical health. Studies show that depression and physical health are closely linked, with one condition potentially exacerbating the other. Below are key ways in which depression can affect physical health:
- Worsening of existing conditions. People with depression often experience worsening symptoms of pre-existing chronic conditions, such as cardiovascular disease, diabetes, and arthritis. Depression can reduce motivation to follow medical recommendations, including taking medication, following a diet, and exercising, which negatively affects the management of these conditions.
- Cardiovascular problems. Research links depression to an increased risk of developing cardiovascular diseases. The stress associated with depression can lead to high blood pressure, worsened atherosclerosis, and an increased risk of heart attacks.
- Immune system. Depression can weaken the immune system, making the body more susceptible to infections and diseases. This can result in an increased frequency and severity of infections, as well as slower recovery times.
- Digestive issues. Depression can cause or worsen digestive problems, such as irritable bowel syndrome (IBS), chronic inflammatory bowel diseases (IBD), and gastroesophageal reflux disease (GERD).
- Pain and chronic conditions. People with depression often report increased sensitivity to pain. This may be related to how depression affects brain chemicals involved in pain signaling. Additionally, depression can worsen the perception of pain in chronic conditions.
- Sleep problems. Sleep disturbances, including insomnia or excessive sleepiness, are common symptoms of depression. Lack of quality sleep can affect physical health, increasing the risk of developing chronic diseases such as obesity, cardiovascular disease, and diabetes.
- Weight gain or loss. Depression can lead to significant changes in appetite, resulting in some people under-eating and losing weight or, conversely, overeating and gaining weight. Both of these conditions can have serious health consequences.
Given the interconnection between depression and physical health, it is important to address both aspects when developing a treatment plan. A comprehensive approach, including treatment for depression and support for physical health, helps improve overall well-being and quality of life.

Myths and Stereotypes about Clinical Depression
There are many misconceptions about clinical depression, which can prevent timely help-seeking and hinder support and understanding from others. Highlighting and discussing these myths helps raise public awareness and create a more supportive environment for those dealing with depression.
- Myth 1: Depression is just a bad mood.
Reality: Clinical depression is a serious medical condition that affects the brain and requires treatment. It is vastly different from ordinary mood swings and can have a profound impact on a person’s daily life.
- Myth 2: Depression is a sign of weakness.
Reality: Depression is not a sign of weakness or a lack of willpower. It is an illness that can affect anyone, regardless of character, willpower, or accomplishments.
- Myth 3: Depression can be overcome through willpower.
Reality: Attempts to overcome depression without professional help are often ineffective and can worsen the condition. Effective treatment usually involves therapy, medication, or a combination of both.
- Myth 4: Depression is a personal problem that doesn’t affect others.
Reality: Depression can have a significant impact on family, friends, and coworkers. Support from loved ones plays a key role in the treatment process.
- Myth 5: People with depression always look sad.
Reality: People with depression may not show visible signs of their condition. Many try to hide their feelings or may appear perfectly fine at work or in social settings.
- Myth 6: Depression never goes away.
Reality: With proper treatment, most people with depression experience significant improvement. Treatment helps manage symptoms and, in many cases, leads to full recovery.
Debunking these and other myths about clinical depression fosters a deeper understanding and empathy for those who suffer from this condition.
The Role of Public Understanding and Support
Public understanding and support play a critical role in the lives of people suffering from clinical depression. In a world where mental health conditions are often stigmatized, raising awareness and empathy can have a significant impact on the recovery and reintegration of people with depression into society.
- Reducing stigma. The fear of stigma is one of the main reasons people with depression may delay or avoid seeking help. Educational programs and awareness campaigns aimed at debunking myths and stereotypes about depression help create a more open and accepting space for discussing mental health. Understanding that depression is a medical condition requiring treatment, not a sign of personal weakness, can encourage more active help-seeking behavior.
- Community support plays a vital role in supporting people with depression by providing resources, information, and access to mental health services. Social groups, hobby clubs, and community organizations are important support networks where people can share their experiences and find understanding.
- Family support. Family plays a central role in the treatment and recovery process for people with clinical depression. Understanding from family members can greatly ease the fight against depression by providing support, motivation, and help with daily tasks, as well as assistance in seeking professional help.
- Workplace and educational institutions. Employers and educational institutions can play an important role in supporting individuals with depression. This could include flexible work schedules or reduced workloads during flare-ups. Understanding and adapting to the needs of people with depression can help them maintain their professional activity and academic success.
- Interaction in the digital space. In the digital age, online communities and social networks can offer additional support and information resources for people suffering from depression. Online platforms can serve as a place to share experiences, receive advice, and connect with others facing similar challenges.
Perspectives on Clinical Depression Research
Research on clinical depression is actively advancing, aiming to improve the understanding of the disease’s mechanisms, develop more effective treatments, and offer personalized approaches to therapy. The scientific community is focused on several key areas that promise significant breakthroughs in the near future.
- Genetic research. Researchers are studying the genetic factors contributing to the development of clinical depression to better understand why some people are more susceptible to the disease than others. Special attention is given to identifying genetic markers that may predict responses to specific treatments, allowing for the development of personalized approaches to therapy.
- Neurobiological research. At the forefront of science are brain studies aimed at exploring the neurobiological foundations of depression. Using advanced technologies such as MRI and PET scans, scientists are trying to identify changes in brain structure and function related to depression, as well as investigate how different brain regions interact in this condition.
- Microbiome research. A growing body of evidence suggests a connection between the gut microbiome and mental health. Researchers are exploring how changes in the gut flora composition may affect the development of clinical depression and other mental disorders, as well as considering potential therapeutic approaches, including probiotics and dietary modifications.
- Development of new therapeutic approaches. The scientific community is actively working on developing new and improving existing methods for treating depression. This includes not only pharmacological treatments but also innovative approaches such as transcranial magnetic stimulation (TMS), deep brain stimulation, and psychedelic therapy.
- Research on psychosocial factors. Important studies are aimed at understanding the role of psychosocial factors in the development of depression. This includes examining the impact of stress, trauma, and socioeconomic conditions, as well as developing effective psychotherapeutic interventions and stress management strategies.
- Research on quality of life. There is increasing focus on research aimed not only at treating depression but also at improving the quality of life for patients, restoring their social adaptation, and professional functions. This involves a comprehensive approach to treatment, including support for a healthy lifestyle, social integration, and professional rehabilitation.
These research directions open new horizons in understanding and treating clinical depression, promising significant improvements in diagnosis, therapy, and support for those suffering from the disease.
Future Treatments and Approaches
The future of treating clinical depression promises to become more personalized and multifaceted, taking into account the unique needs and circumstances of each patient. The development of new approaches and technologies in medicine and psychotherapy is aimed at improving treatment effectiveness and the quality of life for people with depression. Here are some key areas of development for future treatment methods:
- Personalized medicine. The development of more targeted pharmacological agents based on genetic profiles, biomarkers, and individual metabolic characteristics may enhance treatment efficacy and reduce side effects. A personalized approach may also include adapting psychotherapeutic methods to meet the specific emotional and cognitive needs of the patient.
- Innovative pharmacological developments. Neuropharmacology research continues to expand the understanding of the mechanisms behind clinical depression, leading to the development of new medications. Of particular interest is the study of psychedelic substances like psilocybin and MDMA for treating resistant depression, as well as research into how these substances affect brain processes.
- Advancements in neuromodulation technologies. Neuromodulation methods, such as transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), continue to evolve. They can directly impact brain structures and circuits related to depression, offering an alternative to traditional pharmacological and psychotherapeutic approaches.
- Digital technologies and mobile healthcare. The use of digital tools and mobile apps for monitoring health, managing symptoms, and conducting therapy (e.g., through online consultations or meditation apps) is becoming increasingly popular. This not only increases access to care but also allows patients to actively participate in their treatment process.
- Integrative and complementary approaches. The future of treating clinical depression also includes broader recognition and integration of complementary and alternative therapies, such as yoga, meditation, art therapy, and the active use of natural supplements. These approaches can complement traditional treatments to provide a more comprehensive impact on the patient’s condition.
- Social and psychosocial interventions. Improving the quality of life and social support for people with depression remains an important aspect of future treatment approaches. Implementing programs to enhance psychological resilience, social integration, and professional rehabilitation will help strengthen public health and well-being.
Combining these approaches and technologies promises to make the future of clinical depression treatment more effective, accessible, and tailored to the needs of each individual, contributing to faster recovery and improved quality of life.
Recommended Literature
- “The Noonday Demon: An Atlas of Depression” – by Andrew Solomon
This book combines the author’s personal experience with depression and an extensive, thorough examination of the condition. Solomon explores the historical, cultural, biological, and personal aspects of depression, making it comprehensible on multiple levels. - “Feeling Good: The New Mood Therapy” – by David D. Burns
David D. Burns presents a book based on the principles of cognitive therapy, which has helped millions overcome depression without medication. The book offers practical exercises to change the negative thinking patterns that lead to depression. - “Darkness Visible: A Memoir of Madness” – by William Styron
In this memoir, William Styron describes his battle with severe depression. The book is a thoughtful and poignant testimony to his personal experience with the condition. - “An Unquiet Mind: A Memoir of Moods and Madness” – by Kay Redfield Jamison
Kay Redfield Jamison, a professor of psychiatry who suffers from bipolar disorder, shares her experience of living with a serious mental illness. While the book focuses more on bipolar disorder, it provides valuable insights into experiences common to all types of mental illnesses, including depression. - “Lost Connections: Uncovering the Real Causes of Depression – and the Unexpected Solutions” – by Johann Hari
Johann Hari explores the social and cultural causes of depression, moving away from the traditional understanding focused solely on biological factors. The author offers a fresh perspective on the causes and treatment of depression, emphasizing the importance of connection with people and the world around us.
These books provide diverse perspectives on depression, from personal experience and scientific research to innovative ideas about its causes and treatments. They can serve as valuable resources for those dealing with clinical depression or studying it.