Electroconvulsive Therapy (ECT) is a psychiatric treatment method in which a controlled electrical current is passed through the patient’s brain, inducing a brief seizure. Despite its controversial reputation, ECT remains one of the most effective treatments for severe mental disorders such as clinical depression and bipolar disorder.
The history of electroconvulsive therapy dates back to the 1930s when Italian doctors Ugo Cerletti and Lucio Bini first applied this treatment method. They discovered that seizures induced by electrical current could have a therapeutic effect on certain mental disorders. Initially, the procedure was performed without anesthesia or muscle relaxants, which posed risks and discomfort for patients.
Since then, electroconvulsive therapy has undergone significant changes and improvements, becoming a safer and more comfortable procedure. In modern practice, ECT is performed under general anesthesia and with the use of muscle relaxants, minimizing risks and unpleasant sensations for patients.

Indications for Electroconvulsive Therapy
Electroconvulsive therapy (ECT) is one of the most effective methods for treating a range of severe mental disorders. Despite certain concerns and debates surrounding this procedure, it often remains the only viable option for patients with forms of illness resistant to other types of therapy. Indications for ECT are carefully evaluated by clinicians, taking into account the severity of symptoms, the risk to the patient’s life, and the potential response to alternative treatments.
The primary indications for ECT include severe depressive disorders, manic or mixed episodes in bipolar disorder, as well as some other mental disorders resistant to pharmacotherapy. In each case, the decision to administer ECT is made after a thorough analysis of the risks and potential benefits of the procedure for the patient. It is important to note that electroconvulsive therapy is considered only in situations where other treatment options have proven ineffective or are associated with unacceptable side effects.
Severe Depressive Disorders
Electroconvulsive therapy is considered one of the most effective treatments for severe depressive episodes, especially when other therapies, such as antidepressants and psychotherapy, prove ineffective. Studies show that about 50-70% of patients with severe depression respond to ECT, which significantly exceeds the efficacy of pharmacotherapy (20-40%).
The use of ECT in severe depression may be appropriate in the following cases:
- Resistance to antidepressants and other treatment methods;
- Presence of psychotic symptoms, such as hallucinations or delusional ideas;
- High risk of suicide or refusal to eat;
- Need for rapid symptom relief due to the patient’s critical condition.
Bipolar Disorder
Electroconvulsive therapy can be used to treat both manic and depressive episodes in bipolar disorder, especially in cases where traditional pharmacotherapy does not produce the desired results. Research shows that about 70-80% of patients with bipolar disorder respond to ECT.
During a manic episode, electroconvulsive therapy can help quickly stabilize the patient’s condition and eliminate symptoms such as increased activity, sleep disturbances, racing thoughts, and impulsive behavior.
In depressive episodes, electroconvulsive therapy may be used to alleviate severe depressive symptoms when medications prove insufficiently effective or poorly tolerated.
Other Mental Disorders
Electroconvulsive therapy may also be applied in the treatment of some other mental disorders when other treatment methods prove ineffective or have serious side effects. These disorders include:
- Schizophrenia. ECT can be used to treat therapy-resistant cases of schizophrenia, as well as in the presence of catatonic symptoms.
- Catatonia. This severe condition, characterized by motor activity disturbances, can be successfully treated with ECT.
- Severe psychotic disorders. In some cases, electroconvulsive therapy is used to treat psychotic episodes resistant to antipsychotic therapy.
- Postpartum mental disorders. ECT can be effective in severe postpartum disorders, such as postpartum depression or psychosis.
It should be noted that in most cases, electroconvulsive therapy is prescribed only when other treatment methods have proven ineffective or caused serious side effects. The decision to undergo ECT is made individually for each patient, considering the severity of symptoms, risks, and expected benefits of the procedure.

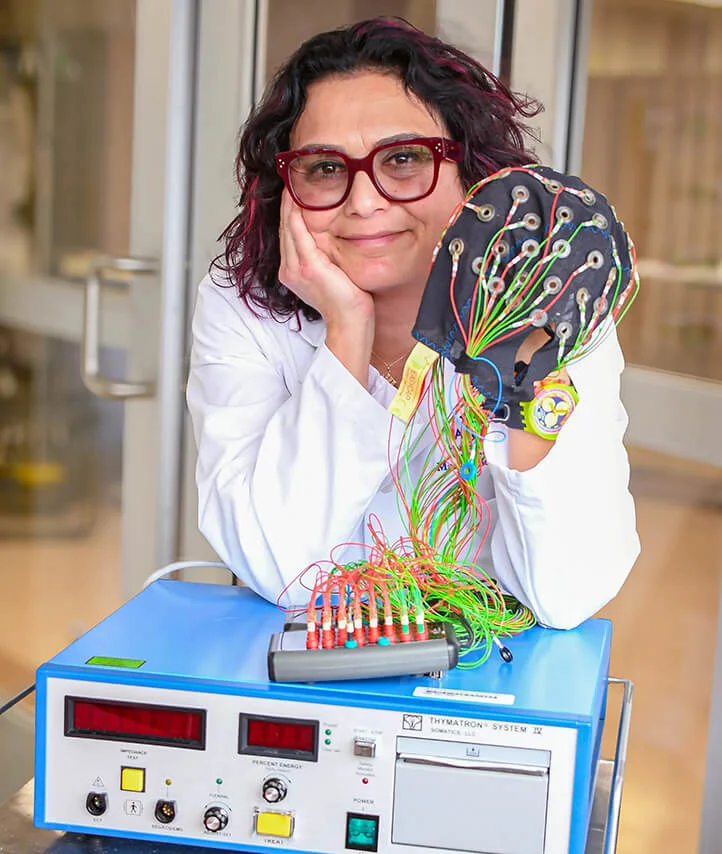
How ECT is Performed
Electroconvulsive therapy is conducted under general anesthesia with the use of muscle relaxants to prevent injury during the induced seizure. Here is a general outline of how the procedure typically occurs:
- Patient preparation. The patient’s vital signs are checked, and necessary anesthesia and muscle relaxation are administered.
- Administration of anesthesia and muscle relaxants. Short-acting anesthetics, such as propofol, and muscle relaxants, such as succinylcholine, are administered to ensure the patient’s safety and comfort during the procedure.
- Passage of an electrical impulse through the brain. Electrodes are placed on the patient’s head, and a controlled electrical impulse is passed through them, causing a brief seizure lasting about 30-60 seconds.
- Monitoring of vital signs. During the procedure, medical staff carefully monitor the patient’s vital signs, including heart rate, blood pressure, oxygen levels, and seizure duration. This ensures the safety of the procedure and allows for immediate intervention if necessary.
- Recovery after the procedure. After ECT is completed, the patient is moved to a recovery area, where medical personnel continue to observe their condition until the anesthesia has completely worn off. Typically, the patient can return home the same day after a few hours of observation.
There are two main types of electrode placement:
- Bilateral electroconvulsive therapy. Two electrodes are placed on either side of the head, and the current passes through both hemispheres of the brain.
- Right unilateral electroconvulsive therapy. One electrode is placed over the right hemisphere, and the other over a part of the skull not associated with the brain. This limits the impact on the left hemisphere and reduces cognitive side effects.
A course of ECT usually consists of 6-12 sessions, conducted 2-3 times a week. The exact number of sessions is determined individually for each patient based on their clinical condition and response to treatment.
Preparation for Electroconvulsive Therapy
Before a course of ECT is prescribed, the patient undergoes a thorough medical examination, which includes:
- Medical history collection and mental health evaluation;
- Physical examination and measurement of vital signs;
- Laboratory blood and urine tests;
- Electrocardiogram (ECG);
- Other diagnostic tests, if required.
This is necessary to identify any potential risks or contraindications for ECT and ensure the procedure’s safety.
Additionally, before starting ECT, the patient must provide informed consent after receiving full information about the risks, benefits, and alternative treatment methods.
Procedure Safety
Modern electroconvulsive therapy is conducted following strict safety protocols. In addition to anesthesia and muscle relaxation, additional safety measures include:
- Use of an oxygen mask to facilitate breathing during the procedure;
- Intravenous administration of a glucose solution to maintain blood sugar levels;
- Application of measures to prevent damage to teeth and tongue during seizures;
- Careful monitoring of vital signs and readiness for immediate intervention if necessary.
Thanks to these precautionary measures, ECT is considered a relatively safe procedure. However, like any medical intervention, it carries certain risks, which will be discussed below.
Mechanism of Action of Electroconvulsive Therapy
Despite the long-standing use of electroconvulsive therapy and its proven clinical efficacy, the exact mechanisms underlying its therapeutic action remain unclear. Scientists have proposed several hypotheses to explain how electrically induced seizures can positively affect symptoms of various mental disorders. Understanding these mechanisms is crucial for further improving ECT methods and enhancing its safety and effectiveness.
Most modern theories agree that electroconvulsive therapy has a complex impact on various neurobiological processes in the brain. It is believed that the seizure caused by the electrical impulse leads to changes in neurotransmitter levels and activity, stimulates processes of neuroplasticity and neurogenesis, and modulates the activity of certain brain regions involved in mood regulation and cognitive functions. A deeper understanding of these mechanisms may pave the way for new advancements in ECT and the development of more targeted and personalized treatments for mental disorders.
Impact on Neurotransmitters and Neuroplasticity
One of the leading hypotheses is that electroconvulsive therapy affects the levels and activity of various neurotransmitters in the brain, such as serotonin, norepinephrine, and dopamine. Changes in these neurotransmitter systems may be associated with improvements in mood and cognitive functions.
Additionally, it is suggested that ECT stimulates neuroplasticity, the brain’s ability to reorganize and form new neural connections. Increased neuroplasticity may help compensate for impaired functions and restore balance in neural networks associated with the development of mental disorders.
Hypotheses on the Antidepressant Effect
One of the most common indications for electroconvulsive therapy is the treatment of severe depressive disorders resistant to other therapies. Numerous clinical studies have demonstrated the high efficacy of ECT in alleviating symptoms of depression, such as low mood, anhedonia, sleep, and appetite disturbances. However, the mechanisms underlying this antidepressant effect are not fully understood, and scientists have proposed several hypotheses to explain them.
Among the most common hypotheses explaining the antidepressant effect of ECT are the neurogenesis hypothesis, the neurotrophic factor hypothesis, and the brain activity alteration hypothesis. Each of these hypotheses focuses on specific neurobiological processes that may be affected by ECT and contribute to the reduction of depressive symptoms.
Neurogenesis Hypothesis
According to this hypothesis, electroconvulsive therapy stimulates the formation of new neurons in the hippocampus, which plays a key role in regulating mood and cognitive functions. Increased neurogenesis may help improve symptoms of depression and cognitive impairments.
Neurotrophic Factor Hypothesis
ECT may increase levels of neurotrophic factors such as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF). These factors are crucial for the survival and functioning of neurons as well as neuroplasticity processes. Raising their levels may contribute to the restoration and strengthening of neural connections disrupted by depression.
Brain Activity Alteration Hypothesis
According to this hypothesis, electroconvulsive therapy alters the activity and metabolism in specific brain regions associated with emotion regulation and cognitive processes, such as the prefrontal cortex, hippocampus, and amygdala. Normalizing activity in these regions may help reduce depressive symptoms and improve cognitive functions.
Although these hypotheses exist, the exact mechanisms of ECT remain unclear, and research in this area continues. However, the existing data suggest that electroconvulsive therapy exerts a complex influence on various neurobiological processes, which together may significantly enhance its therapeutic effect.

Side Effects and Risks
Like any medical procedure, electroconvulsive therapy (ECT) is associated with certain side effects and health risks for patients. Despite significant improvements in the technique of administering ECT and safety measures, it is impossible to completely eliminate unwanted consequences. Understanding potential side effects is crucial for making an informed decision regarding the use of ECT in each individual case.
The most common side effects of electroconvulsive therapy are temporary cognitive impairments, such as memory problems, difficulties with concentration, and learning issues. In addition, some patients may experience headaches, muscle pain, or numbness after the procedure.
There are also certain risks related to the use of anesthesia, which is required for ECT. Understanding the nature, severity, and duration of these side effects allows the medical team to develop appropriate strategies for minimizing and managing them.
Temporary Cognitive Impairments
One of the most common side effects of ECT is temporary memory and cognitive function impairment. These impairments can include:
- difficulties remembering recent events (retrograde amnesia);
- problems with concentration and slower thinking;
- challenges in learning and retaining new information.
The degree and duration of cognitive impairments can vary from mild to moderate and depend on several factors such as:
- the type of electroconvulsive therapy (bilateral or right unilateral);
- the number of ECT sessions in the course;
- the individual characteristics of the patient.
In most cases, cognitive functions recover within a few weeks or months after the end of the ECT course. However, in some cases, persistent memory impairments may occur, particularly regarding events that happened before the treatment (retrograde amnesia).
To minimize cognitive side effects, right unilateral ECT is often recommended instead of traditional bilateral ECT, as well as conducting fewer procedures in the course once the desired therapeutic effect is achieved.
Headaches and Muscle Pain
Some patients may experience headaches, muscle pain, or numbness after ECT. These side effects are usually mild and resolve on their own within a few hours or days after the procedure.
Pain relief medications may be prescribed to alleviate these symptoms. Additionally, the use of modern anesthesia and muscle relaxation methods helps prevent muscle injuries and related pain.
Risks Related to Anesthesia
Since electroconvulsive therapy is performed under general anesthesia, there are risks associated with the use of anesthetics. These risks include:
- allergic reactions to anesthetics;
- breathing problems and oxygen saturation issues;
- cardiovascular complications such as arrhythmias or changes in blood pressure;
- nausea and vomiting after recovering from anesthesia.
However, modern anesthesia methods and thorough pre-procedure medical evaluations help reduce these risks to a minimum.
Other Possible Side Effects
Other potential side effects of electroconvulsive therapy include:
- confusion and disorientation after the procedure (usually temporary);
- speech and swallowing difficulties (rare);
- increased fatigue and drowsiness;
- higher risk of falls;
- hypomanic or manic episodes (rare).
Most of these side effects are temporary and subside as the ECT course concludes and the body recovers.
Before prescribing ECT, the physician must carefully evaluate the potential risks and benefits of the procedure for the specific patient. In some cases, side effects may outweigh the expected benefits, and alternative treatment methods should be considered.

Effectiveness of Electroconvulsive Therapy
One of the key factors determining the appropriateness of using ECT to treat various mental disorders is its proven clinical efficacy. Over decades, numerous scientific studies have confirmed that electroconvulsive therapy is one of the most effective treatment methods in cases of resistance to pharmacological treatment and psychotherapy.
The level of ECT effectiveness can vary depending on the specific disorder and individual patient characteristics. Nevertheless, aggregated data indicate a high likelihood of a positive response to treatment, often surpassing the results of alternative therapies. Additionally, electroconvulsive therapy can provide more rapid symptom relief, which is crucial in critical situations such as a high risk of suicide or sudden deterioration in the patient’s condition.
Long-term Results and Relapses
While electroconvulsive therapy is an effective method for treating acute symptoms of mental disorders, there is a risk of relapse after completing the therapy course. To maintain long-term results, ongoing pharmacotherapy or additional ECT courses are often required.
Nevertheless, many patients report prolonged improvement after undergoing ECT. Some studies show that about 50% of patients with depression remain in remission for one year after ECT, while for bipolar disorder, this figure is around 60%.
It is important to note that long-term outcomes largely depend on individual patient characteristics, the severity of the condition, and subsequent maintenance treatment. Regular follow-up with a doctor and timely adjustments to the therapy help extend the remission period and prevent relapses.

Modern Developments and Modifications of ECT
Since its discovery in the 1930s, the method of electroconvulsive therapy (ECT) has undergone numerous changes and improvements. In an effort to increase the effectiveness and safety of this procedure, scientists and clinicians have continuously sought new approaches and modifications. In recent decades, research in the field of ECT has led to several promising developments that could significantly improve treatment outcomes and reduce the risk of unwanted side effects.
One of the most important areas of modern research is increasing the precision and selectivity of targeting specific areas of the brain. Traditional methods of ECT are characterized by relatively broad and non-specific propagation of the electrical impulse, which can lead to unwanted side effects. New developments, such as ultrabrief pulse electroconvulsive therapy, magnetic seizure therapy, and right unilateral electroconvulsive therapy, aim for more precise and localized stimulation, which may improve treatment outcomes and minimize cognitive impairments.
Right Unilateral Electroconvulsive Therapy
Traditionally, electroconvulsive therapy is performed using a bilateral electrode configuration, where the electrical impulse spreads across both hemispheres of the brain. However, in recent years, right unilateral ECT has been increasingly used, where one electrode is placed over the right hemisphere.
The advantage of this modification lies in reducing cognitive side effects, as the left hemisphere, responsible for many cognitive functions, is not directly affected by the electrical current. Studies show that right unilateral ECT can be as effective as bilateral ECT, but with a lower risk of memory and concentration impairments.
Ultrabrief Pulse Electroconvulsive Therapy
Traditional electroconvulsive therapy uses electrical pulses lasting about 1 millisecond. However, some research suggests that the use of ultrabrief pulses (in the range of 0.3-0.5 milliseconds) can be just as effective but with fewer side effects, including cognitive impairment.
It is believed that ultrabrief pulses cause more localized and selective activation of neurons in specific brain regions associated with mood regulation and cognitive functions. This allows for a therapeutic effect with less overall impact on the brain.
Magnetic Seizure Therapy (MST)
MST is a new modification of electroconvulsive therapy in which a powerful magnetic field is used to induce a seizure instead of electrical current. This allows for more precise targeting of specific areas of the brain while minimizing side effects.
The benefits of MST include the absence of a need for anesthesia, fewer cognitive disturbances, and potentially higher effectiveness due to localized stimulation. However, this technology is still in active research, and more data is needed to determine its long-term efficacy and safety.
Low-Frequency Electroconvulsive Therapy
Traditional ECT is typically performed at a frequency of around 60-120 Hz. However, some researchers are exploring its application at lower frequencies (in the range of 0.5-2 Hz) to reduce the number of seizures and associated side effects.
Low-frequency electroconvulsive therapy may be especially useful for elderly patients or those with comorbid conditions who tolerate seizures poorly. Although data on the efficacy of this modification is still limited, it represents an area of interest for further research.
Combination Therapy
In some cases, electroconvulsive therapy can be used in combination with other treatment methods, such as pharmacotherapy or psychotherapy. This combined strategy enhances overall treatment effectiveness and reduces the risk of relapse after the ECT course.
For example, taking antidepressants or mood stabilizers during and after the ECT course may help consolidate and prolong the therapeutic effect. Additionally, psychotherapy can contribute to further improvement and the development of skills to cope with symptoms after completing ECT.
The choice of the optimal combination of treatment methods is individualized for each patient, taking into account their clinical picture, preferences, and response to previous types of therapy.
Thanks to ongoing research and development, electroconvulsive therapy continues to evolve, becoming a safer, more effective, and more personalized procedure for the treatment of various mental disorders.

Ethical Aspects and Perception of Electroconvulsive Therapy
Despite the proven effectiveness of electroconvulsive therapy in treating several severe mental disorders, this procedure remains one of the most controversial and debated topics in psychiatry and medical ethics. Over the years, ECT has faced significant criticism and concerns regarding its impact on patients’ autonomy and dignity, as well as potential human rights violations.
The roots of these concerns lie in the early history of ECT when the procedure was often performed without proper anesthesia, muscle relaxation, or informed consent from patients. This led to the widespread negative perception and stigmatization of ECT in the public consciousness. Even with significant improvements in technique and adherence to ethical standards, certain prejudices and disputes about ECT persist, which need to be addressed.
Ongoing Concerns and Stigmatization
One of the main reasons for the negative perception of ECT is its history and methods used in the past. In its early development, electroconvulsive therapy was performed without proper anesthesia and muscle relaxation, which could lead to injuries and unpleasant sensations for patients. Additionally, in some cases, the procedure was applied coercively, without the patient’s informed consent.
These factors contributed to the spread of negative stereotypes and the stigmatization of ECT in society, which persist today despite significant improvements in the procedure and ethical standards.
Concerns are also related to the potential side effects of ECT, particularly cognitive impairments, which may be perceived as a violation of the patient’s personal integrity and autonomy.
Informed Consent and Patients’ Rights
In modern practice, electroconvulsive therapy is performed in compliance with strict ethical standards and requirements, including obtaining informed consent from the patient or their legal representative. Patients must be fully informed about the procedure, its risks, potential benefits, and available alternatives.
However, in some cases, disputes arise about whether a patient with a severe mental disorder, such as major depression or psychosis, can give valid informed consent. These conditions may impair the ability to make considered decisions and adequately assess the risks and benefits of treatment.
To address this issue, many countries have enacted laws and regulations governing the use of ECT. Typically, for patients unable to give informed consent, the approval of a legal representative (guardian) or a special ethics committee is required.
Furthermore, electroconvulsive therapy should only be used when the expected benefit to the patient significantly outweighs the potential risks, and other treatment methods have proven ineffective.
Respecting the Autonomy and Dignity of the Patient
In addition to obtaining informed consent, it is important to ensure respect for the autonomy and dignity of the patient at all stages of the ECT process. This includes:
- Providing complete information about the procedure and its alternatives;
- Allowing the patient to refuse treatment or discontinue it at any time;
- Ensuring the confidentiality of medical data;
- Maintaining respectful and humane treatment from the medical staff.
Patients should have the opportunity to actively participate in decision-making about their treatment and express their concerns and preferences.
Overcoming Stigmatization
Despite efforts to improve the practice, the stigmatization of ECT remains a significant barrier to its wider acceptance. Many patients and their families fear negative societal attitudes and judgment, which can deter them from opting for this effective treatment method.
To overcome stigmatization, public awareness of modern methods of ECT, its effectiveness, and its safety when ethical standards are followed must be increased. It is important to dispel myths and outdated perceptions of electroconvulsive therapy based on inaccurate or biased information.
Additionally, access to quality education and support for patients and their families should be ensured so they can make informed treatment decisions based on facts rather than fears and prejudices.
Overcoming the stigmatization and ethical issues related to ECT requires ongoing efforts from the medical community, governmental bodies, patient rights organizations, and society itself. Only through open dialogue and adherence to strict ethical standards can this important treatment method be made accessible and acceptable to those who need it.
Conclusion
Electroconvulsive therapy remains one of the most effective methods for treating severe mental disorders such as depression, bipolar disorder, schizophrenia, and other conditions resistant to traditional pharmacotherapy. Despite some side effects and ethical controversies surrounding ECT, its benefits often outweigh the risks for patients with severe forms of illness.
In modern clinical practice, electroconvulsive therapy is performed in accordance with strict safety and ethical protocols, including obtaining informed consent, ensuring anesthesia, and monitoring vital signs. Moreover, various modifications of ECT have been developed to improve effectiveness and reduce side effects.
Despite these efforts, concerns and stigmatization surrounding electroconvulsive therapy persist, rooted in its history and outdated perceptions. Overcoming these barriers requires continuous public education, adherence to ethical principles, and respect for the rights and dignity of patients.
In the future, further advancements in ECT methods are expected, with the goal of enhancing efficacy, safety, and the individualization of treatment. Researchers continue to explore new modifications of the procedure, as well as long-term outcomes and strategies for maintaining remission after an ECT course.