Fatal familial insomnia (FFI) is a rare hereditary neurodegenerative disorder characterized by a progressive loss of the ability to sleep, mental function disturbances, and other neurological symptoms. This disease is caused by mutations in a specific gene responsible for the creation of a particular protein in the body, known as a prion protein.
The disease occurs in 1-2 people per million, manifests in adulthood, most often between the ages of 30 and 60, and usually leads to death within a few months or years after the onset of the first symptoms.
It is important to note that there is currently no effective treatment for fatal familial insomnia. Therefore, the primary efforts of specialists are aimed solely at alleviating symptoms and maintaining the quality of life of patients.
The disease does not have a specific geographic distribution. To date, cases have been reported in various countries and regions worldwide. The term “familial” in the name of the disease indicates its hereditary nature. This implies that the mutation causing the disease is passed from parents to children.
If there have been cases of this disease in a family, the risk of its occurrence in subsequent generations increases significantly. This characteristic makes it important to study the family medical history when assessing the risk of developing fatal familial insomnia in a specific individual.
Currently, no significant influence of gender or ethnicity on the likelihood of developing FFI has been found. However, the limited data may be due to the difficulty in diagnosing and recording cases of the disease.

Fatal Familial Insomnia: A Historical Overview
The first records of fatal familial insomnia date back to the mid-20th century when unusual cases of insomnia accompanied by a range of other symptoms began to be discussed in medical circles. These early cases became the starting point for decades of scientific research by scientists worldwide, who sought to unravel the complex network underlying this astonishing and simultaneously frightening disease.
In the 1990s, researchers made a significant breakthrough in understanding the nature of this disease. They discovered that the cause of fatal familial insomnia is mutations in a specific gene responsible for the creation of a specific protein—a prion. This discovery not only uncovered the genetic basis of the disease but also pointed to a connection with other prion diseases, suggesting new directions for research in this area.
Over time, it became clear that fatal familial insomnia is not just a sleep-related disorder but a broader neurological disorder that affects many aspects of patients’ lives.
To this day, the scientific community continues to work on finding effective methods for treating and alleviating the symptoms of fatal familial insomnia, giving hope to those who face it.
The Evolution of Medical Understanding of the Disease
The evolution of medical understanding of fatal familial insomnia can be divided into several key stages:
- Early Stage (Mid-20th Century)
- Initial Observations: The first cases of the disease were recorded and described as abnormal cases of insomnia accompanied by neurological symptoms.
- Recognition of the Disease’s Uniqueness: Over time, the medical community began to realize that they were facing a new, previously unknown disease.
- Period of Intensive Research (1980s – 1990s)
- Genetic Research: During this period, research in genetics began to develop actively, allowing the establishment of the genetic nature of the disease.
- Discovery of the Prion Theory: In the 1990s, the prion theory was proposed, which explained the mechanism of disease transmission through abnormal proteins.
- Modern Stage (2000s – Present)
- Expanding Knowledge of Clinical Manifestations: The scientific research community continues to work on detailing the clinical manifestations of the disease and methods for its diagnosis.
- Development of Therapy: Currently, scientists are actively working on developing methods for treating and preventing fatal familial insomnia, including anti-prion therapy and genetic interventions.
Pathophysiology of Fatal Familial Insomnia
Fatal familial insomnia (FFI) is one of the most mysterious and least understood diseases of modern times. It is a rare hereditary neurodegenerative disorder that remains a subject of active research.
The complexity of the disease lies in its pathophysiology, which is based on the accumulation of misfolded prion proteins in the nervous system, leading to neuronal death and disruption of normal brain function.
To understand how mutations in a specific gene can cause such dramatic and tragic consequences for patients and their families, it is necessary to delve into the world of molecular biology.
Analyzing the pathophysiological aspects of fatal familial insomnia not only allows us to understand the mechanisms of disease development but also, potentially, to find ways for effective treatment in the future. This is an important step toward a deeper understanding and possible control of one of the most complex medical mysteries of our time.
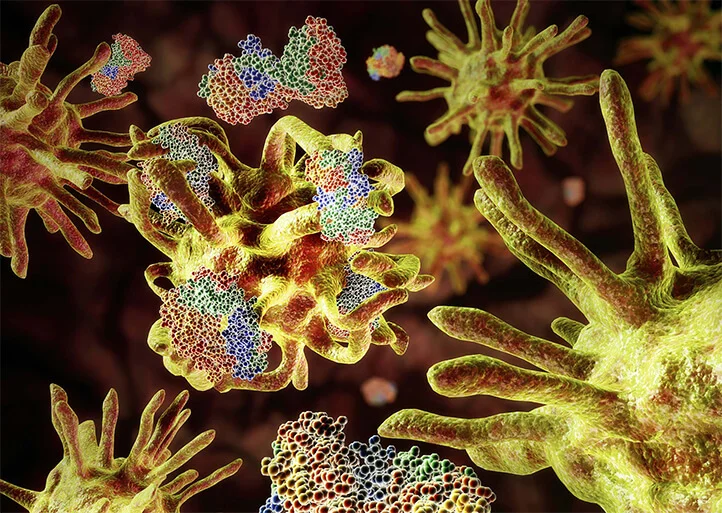
Prion Proteins
Prion proteins are a special category of proteins that can acquire abnormal structural forms, placing them at the center of a number of neurodegenerative diseases, including fatal familial insomnia. These proteins can cause similar abnormal structural changes in normal molecules of the same protein, creating a chain reaction that leads to the accumulation of toxic forms of the protein in the brain.
In their proper state, prion proteins, known as PrPC, are components of the cell membrane and perform various functions related to cell protection and signaling. However, under certain conditions, such as mutations in the PRNP gene (which encodes the prion protein), these proteins can adopt an abnormal form, referred to as PrPSc. This form is highly resistant to degradation and has the ability to induce structural changes in normal protein molecules, leading to the formation of protein aggregates or plaques that are toxic to nerve cells.
Understanding the mechanisms of interaction between prion proteins, their structure, and functions is key to developing strategies for diagnosing and treating prion-related diseases, such as fatal familial insomnia.
Impact on the Nervous System
Fatal familial insomnia has a profound impact on the nervous system, primarily affecting brain structures responsible for regulating sleep and various cognitive functions. Here’s how this impact unfolds:
- Accumulation of Prion Proteins: Abnormal prion proteins begin to accumulate in brain tissues, forming aggregates that damage neurons. This occurs due to their ability to alter the structure of normal protein molecules, leading to a chain reaction of accumulating toxic protein forms.
- Neurodegeneration: A gradual destruction of nerve cells or neurons in specific areas of the brain. This process is accompanied by the deterioration of neuronal connections, which disrupts the normal functioning of the nervous system.
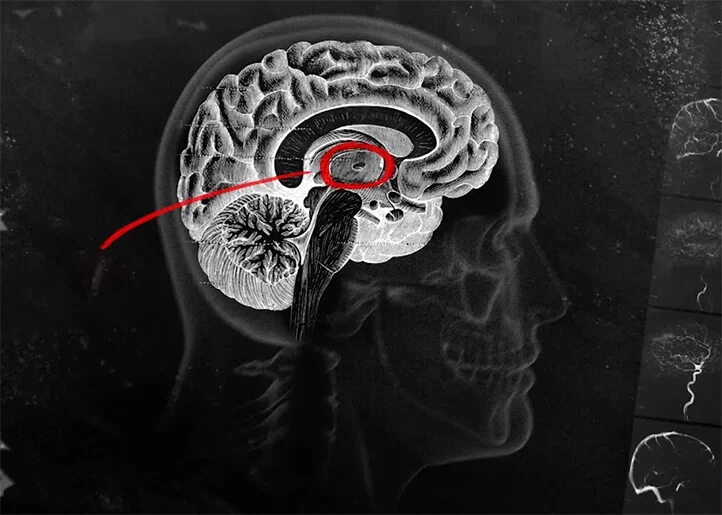
- Impact on the Thalamus and Hypothalamus: Particular impact is exerted on the thalamus (involved in regulating consciousness, sleep, and wakefulness) and the hypothalamus (responsible for many vital functions, including sleep-wake cycles). Damage to these areas can explain symptoms of insomnia and cognitive impairment.
- Psychiatric and Behavioral Changes: Due to the damage to the nervous system, patients may experience a range of psychiatric and behavioral changes, including depression, anxiety, hallucinations, and personality changes.
- Sleep Disorders: Fatal familial insomnia is characterized by sleep disturbances, including chronic insomnia, which is associated with damage to brain structures that regulate the sleep-wake cycle.
- Lethal Outcome: Unfortunately, the disease progresses to a stage where the patient’s body can no longer function normally, ultimately leading to death, usually within months or years after the onset of the first symptoms.

Symptoms of Fatal Familial Insomnia
Fatal familial insomnia most prominently manifests as chronic sleep disruptions. However, the spectrum of symptoms of this disease is much broader, including a range of neurological and psychiatric manifestations. From a pathophysiological perspective, these symptoms are associated with the gradual accumulation of abnormal prion proteins in the brain, leading to irreversible neuron damage. Understanding this disease begins with awareness of the diversity of its symptoms, which can vary from case to case.
The initial signs of fatal familial insomnia are often perceived as ordinary sleep disorders. Patients may complain of increased insomnia, unusual dreams, or even a complete lack of sleep. Over time, however, these symptoms become more extreme, taking on the characteristics of a true battle with insomnia that disrupts the normal rhythm of a person’s life.
As the disease progresses, other neurological symptoms appear, such as motor impairments in the form of involuntary movements, tremors, or persistent muscle tension. Concurrently, patients may develop cognitive impairments, such as memory loss and reduced concentration, which worsen over time, decreasing the quality of life.
It is important to note that fatal familial insomnia also affects the mental state of patients. The appearance of signs of depression, anxiety, apathy, or even psychotic symptoms, such as hallucinations, is not uncommon. This highlights the multifaceted impact of the disease on the human body and the need for a comprehensive approach to its study and treatment.
Early Symptoms
In the early stages of fatal familial insomnia, symptoms may be relatively subtle or mistakenly attributed to other, less serious conditions. In most cases, the disease manifests through sleep disturbances. Patients may notice problems falling asleep, frequent awakenings at night, or increased daytime fatigue due to a lack of quality sleep.
Over time, other early symptoms may also appear, including strange or vivid dreams, as well as minor changes in behavior or mood. Cognitive functions, such as memory and concentration, may also be slightly affected. During this period, it is important to closely monitor the dynamics of the condition, as early detection can significantly help in supporting the patient.
Disease Progression
As fatal familial insomnia progresses, the patient’s condition begins to deteriorate exponentially. Initially, sleep disturbances become more pronounced, turning into chronic insomnia. Patients lose the ability to fully rest during sleep, which significantly affects their overall physical and mental well-being.
Simultaneously with the deterioration of sleep quality, there is an intensification of neurological symptoms. Motor disorders may occur, such as tremors, muscle tension, and slowed movements. Cognitive functions continue to deteriorate, affecting memory, attention, and learning ability. Patients face increasing difficulties in performing daily tasks and a decline in their quality of life.
Over time, patients may also experience severe psychiatric changes, including depression, apathy, as well as psychotic symptoms such as hallucinations and delusions. This makes the disease particularly distressing not only for patients but also for their families and loved ones.
In the final stage of the disease, patients lose the ability to function independently, requiring round-the-clock care.
Unfortunately, at present, fatal familial insomnia remains an incurable disease that ultimately leads to death. However, scientific research in this field continues with the aim of finding effective treatment methods or, at the very least, ways to slow the progression of the disease.
Diagnosis of Fatal Familial Insomnia
The diagnosis of fatal familial insomnia (FFI) is a critical step in managing this rare but severely debilitating disease. Documented cases within certain families highlight the need for thorough medical examinations and genetic testing when there is a relevant family history. Initially, doctors may focus on patients’ complaints of chronic insomnia and other neurological symptoms that could indicate the presence of the disease.
The diagnostic process involves various methods, including neuroimaging studies such as MRI or CT scans of the brain to assess potential structural damage. Electroencephalography (EEG) can also be useful for analyzing brain electrical activity, which may be disrupted in this condition. In addition, laboratory tests may be conducted to evaluate other possible conditions in the patient.
The primary challenge in diagnosing FFI lies in the fact that many of its symptoms often overlap with other neurological or psychiatric disorders. This creates a need for a comprehensive approach, including a thorough analysis of family history and the potential use of genetic testing to identify characteristic mutations in the PRNP gene.
Genetic testing, in particular, plays a central role in diagnosing this condition by identifying mutations associated with FFI. Detecting these mutations aids in establishing a diagnosis and planning further patient care. The involvement of specialists from various medical fields, including neurologists, psychiatrists, and geneticists, ensures the most comprehensive and accurate diagnosis, which is crucial for the disease management strategy.
Diagnostic Methods
Diagnostic methods for fatal familial insomnia involve a complex set of procedures designed to detect the presence of this rare disease. Here are some key methods that may be employed in this process:
- Clinical Examination: In the initial phase of diagnosis, doctors conduct a thorough clinical examination, including taking a family history, to determine potential risks for developing the disease.
- Neuroimaging (MRI or CT): Used to visualize brain structures and detect potential abnormalities or changes associated with disease progression.
- Electroencephalography (EEG): Can be applied to analyze brain electrical activity, which is often disrupted in this condition.
- Lumbar Puncture: Useful for analyzing cerebrospinal fluid for proteins associated with prion diseases.
- Genetic Testing: A key method for identifying mutations in the PRNP gene, which is the primary cause of FFI.
- Polysomnography: This test is used to monitor various physiological parameters during sleep and can help diagnose sleep disturbances characteristic of the disease.
- Neuropsychological Testing: Helps assess the disease’s impact on cognitive functions, including memory, attention, and other aspects of mental activity.
- Biochemical Blood Tests: May be conducted to assess the patient’s overall health and identify other possible diseases.
This set of methods allows doctors to diagnose fatal familial insomnia with a high degree of probability and develop a disease management strategy.
Differential Diagnosis
Differential diagnosis is a crucial stage in diagnosing fatal familial insomnia. This process involves medical professionals trying to distinguish this disease from other conditions with similar symptoms.
- Symptom Assessment: Analyzing and comparing the symptoms of FFI with those of other neurological or psychiatric diseases.
- Exclusion of Other Diseases: In this process, doctors exclude other possible diseases based on clinical manifestations and diagnostic findings.
- Comparison with Other Prion Diseases: Investigating the possibility of other prion diseases, such as Creutzfeldt-Jakob disease, which have similar neuropathological characteristics.
- Analysis of Family History: Helps distinguish FFI from other hereditary or familial neurological conditions.
- Use of Specialized Diagnostic Tests: Including genetic testing for accurate disease identification.
- Consultations with Specialists: Involving neurologists, psychiatrists, and geneticists to ensure a multidisciplinary approach to diagnosis.
- Serendipitous Findings During Research: Occasionally, unexpected findings during studies can help differentiate FFI from other conditions.
By gathering all the data and conducting a thorough evaluation, medical professionals can make the most accurate diagnosis, which is crucial for determining the best course of treatment and care for the patient.

Impact on Patients and Their Families
Fatal familial insomnia not only relentlessly affects the physiological condition of patients but also has a significant impact on the psycho-emotional state of their loved ones. Families facing this disease often encounter numerous challenges, from finding adequate medical care to adapting to new, more complex life circumstances.
The disease inevitably introduces elements of uncertainty and anxiety into the daily lives of families. The ability to maintain normal relationships may weaken, as caring for a patient requires considerable effort and time. This can provoke conflicts, stress, and even depression among family members who feel physical and emotional exhaustion.
A diagnosis of FFI often causes shock and denial reactions, both in the patient and their loved ones. The process of accepting the new reality may take a long time, during which psychological support and counseling are necessary. Maintaining optimism and hope in such moments can become a real challenge.
Nevertheless, many families find ways to adapt and overcome the challenges posed by the disease. The importance of family support and solidarity cannot be underestimated, as together they sustain the patient’s quality of life and preserve family unity.
Psychosocial Aspects
The psychosocial aspects of fatal familial insomnia cover a wide range of issues, including the mental health of patients and their families, as well as their social interactions. Individuals with this disease may experience various psychological problems, including anxiety, depression and despair. In addition, families may face social rejection, discrimination, and financial difficulties.
Individual and Family Coping Strategies include psychotherapy, support groups, and other methods of psychosocial assistance. Families may find support and comfort in communities of people with similar problems, where they can exchange experiences and strategies for living with the disease.
An important aspect is also public awareness of the disease. This may include educational programs aimed at reducing discrimination and promoting social integration of patients.
Overall, the psychosocial aspects of fatal familial insomnia require a multifaceted approach, including both individual psychotherapeutic support and broad community initiatives.

Treatment and Care for Fatal Familial Insomnia
Unfortunately, there is currently no known cure for this disease, but active scientific research continues in search of effective methods and potential medications.
As the disease progresses, it becomes increasingly important for patients and their families to focus on quality care and supportive measures that help alleviate the physical and psychological suffering associated with the progression of the disease, as well as on the available medical and social resources that can assist both patients and their families.
Current Treatment Methods
As of the writing of this article, scientists and medical professionals are still exploring and testing potential treatments for fatal familial insomnia. Unfortunately, no specific therapy has been developed to fully cure or halt the progression of this disease.
In medical practice, current treatments are primarily aimed at symptom relief and improving patients’ quality of life, including medication to manage specific symptoms such as insomnia, anxiety, or depression.
Significant attention is also given to supportive therapy, in which specialists help patients maintain an optimal level of physical activity and nutrition, as well as provide psychological support to cope with the emotional and psychosocial aspects of the disease.
An important part of assistance from medical personnel is involving family members and loved ones in the process of learning proper care for the patient and providing support to overcome emotional stress. Family counseling and support groups play a significant role in this process.
Supportive Care and Palliative Care
Supportive care and palliative care play a vital role in managing fatal familial insomnia. Given the absence of a specific cure, the goal of these approaches is to minimize patient suffering and improve their quality of life at various stages of the disease.
Supportive care includes various aspects, such as maintaining physical activity at the highest possible level, ensuring adequate nutrition, and helping manage daily tasks and activities. Specialized therapies, such as physical therapy or occupational therapy, can be integrated into the care plan to maintain functionality and independence for as long as possible.
On the other hand, palliative care focuses on alleviating suffering and improving patients’ quality of life primarily through managing pain and other severe symptoms, such as insomnia or anxiety. This may involve using both pharmacological and non-pharmacological methods to control symptoms.
Another important aspect is the psychosocial support for patients and their families. The disease imposes a significant emotional and psychological burden on all involved in the care process, and psychological assistance is an invaluable resource during this challenging time.
Organizing support for families, providing information and resources, and assisting in planning future care are valuable components of a comprehensive strategy for managing this disease.
Scientific Research and Future Perspectives
Today, scientists are actively studying the molecular and genetic aspects of the disease to better understand its nature and find ways to control or prevent it.
A lot of attention is being given to studying prion proteins, which play a key role in the development of the disease. Scientists hope that by conducting a detailed analysis of these proteins, they may develop strategies to block or slow the progression of fatal familial insomnia.
In addition, research is underway to develop new diagnostic methods that would allow for earlier detection of the disease, which could significantly improve the prognosis and quality of life for patients.
However, despite the ongoing active scientific search and significant investment in research, the path to developing an effective treatment remains long and challenging. Nevertheless, with each passing year, scientists are getting closer to achieving this goal, continuing to hope and work toward creating a brighter future for patients with fatal familial insomnia.




