Imagine a person who intentionally induces symptoms of illnesses in themselves, endures painful medical procedures, and switches hospitals one after another. This is not about a desire for sick leave or insurance—something much more complex and profound drives these people. Münchausen syndrome, one of the most enigmatic mental disorders of modern times, continues to baffle doctors and researchers despite decades of study.
The History of Münchausen Syndrome
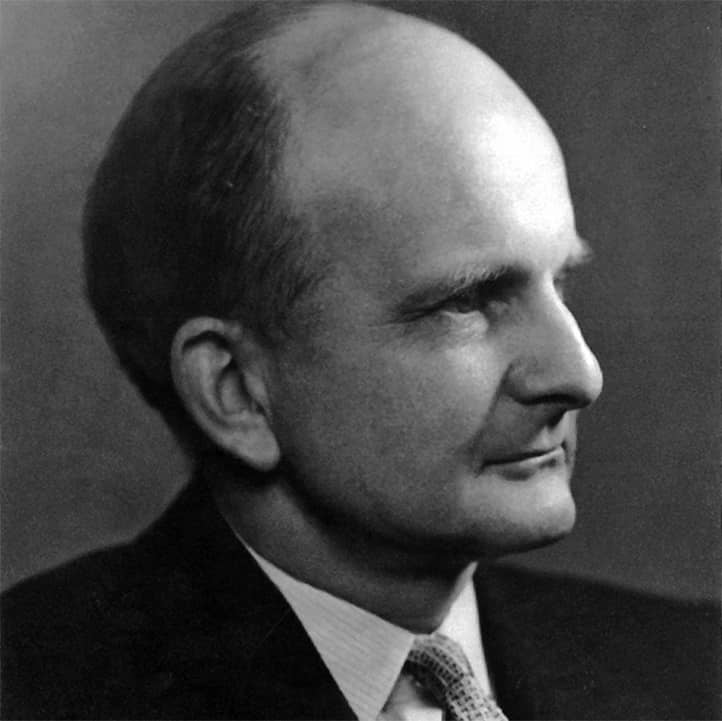
The origin of this disorder dates back to the 18th century and is associated with the name of Baron Karl Friedrich Hieronymus von Münchausen. This German military officer became famous for his incredible tales of military exploits and adventures, so fantastical that his name became synonymous with someone prone to exaggerations and fabrications.
In 1951, British endocrinologist Richard Asher first described a group of patients who deliberately produced symptoms of various diseases. Drawing a parallel between their behavior and the Baron’s famous tales, he named this condition Münchausen syndrome. Asher’s publication in the prestigious medical journal The Lancet initiated the systematic study of this disorder.
Since then, the understanding of Münchausen syndrome has undergone significant evolution. In the 1970s, a specific manifestation was described—Münchausen syndrome by proxy, in which a caregiver induces or fabricates illness in another person, typically a child. With the rise of the internet, a new form of the disorder emerged—virtual Münchausen syndrome, where people create stories about severe illnesses on social media.

Clinical Picture of the Disorder
Münchausen syndrome manifests as a complex array of symptoms and behavioral patterns. Foremost among them is the pathological drive toward medical procedures. Patients are frequently hospitalized, insistently demand various interventions, and are constantly seeking new treatment methods. They demonstrate a remarkably deep knowledge of medicine, easily use technical terminology, and can describe symptoms of various diseases in detail.
A notable characteristic of these patients is their tendency to dramatize their condition. They can spend hours recounting their suffering, with stories that sound convincing and emotionally charged. However, when attempts are made to verify the facts or suggest psychiatric consultation, they often resist and may disappear, only to reappear at another hospital with a new illness story.
The classic form of Münchausen syndrome is characterized by the patient’s direct actions upon their own health. People may inject themselves with various substances, intentionally infect wounds, or interfere with the healing process. They may simulate a wide range of conditions: from acute pain to neurological symptoms and mental disorders, showing remarkable inventiveness in creating and sustaining symptoms.

Münchausen Syndrome by Proxy
Münchausen syndrome by proxy, also known as factitious disorder imposed on another, is a form of the disorder in which a person fabricates or induces illness in another individual, most often a dependent, such as a child. Typically, the “agent” is the mother, who actively manages the child’s medical care, inventing or artificially inducing symptoms. This phenomenon was first described in 1977 by British pediatrician Roy Meadow and has since been a subject of active study.
The main feature of Münchausen syndrome by proxy is that the perpetrator intentionally harms another person to gain attention and sympathy from medical professionals. Parents, often mothers, may administer toxic substances to the child, simulate symptoms of infectious diseases, or insist on unnecessary medical procedures. In most cases, this is done covertly, making diagnosis particularly challenging.
For healthcare providers, this syndrome presents a unique challenge, as the child cannot independently describe their symptoms, and the parent responsible for their health is generally seen as a reliable source of information. Numerous cases of this syndrome were only discovered after years of manipulation, resulting in severe physical and psychological consequences for the child. Without medical intervention, the mortality rate among children subjected to such abuse can reach 10%.
Diagnosis of Münchausen syndrome by proxy requires collaboration among various specialists: pediatricians, psychologists, and social workers. The primary diagnostic method involves careful observation of how symptoms manifest in the presence or absence of the parent, along with cross-referencing data from multiple medical institutions. Key indicators include:
- Symptoms that cannot be explained by conventional medical tests.
- Lack of improvement in the child’s condition despite treatment.
- Excessive interest by the parent in medical procedures.
- Frequent visits to different medical facilities without completing treatment.
- Conflicting reports from different doctors and medical centers.
Treatment for Münchausen syndrome by proxy includes both protecting the child from further harm and providing psychiatric help to the parent with the disorder. The primary task for medical professionals is to establish clear boundaries, restricting the parent’s access to the child under medical supervision, followed by developing a comprehensive psychotherapy program for the perpetrator.

Recent Research and New Forms of the Disorder
In recent years, researchers have increasingly focused on the phenomenon of “digital Münchausen syndrome.” With the advent of social media, new platforms have emerged for expressing this disorder. Patients create detailed online personas with fictitious illness stories, blog about their “struggle with the disease,” and gather support communities around them. This phenomenon is known as “illness faking online” (IFO) or “digital factitious disorder.”
A particular concern is that the virtual form of the disorder may be a precursor to the development of classic Münchausen syndrome. Studies indicate that around 30% of patients with a confirmed diagnosis started by creating fake illness stories online before moving to physical symptom simulation.
The COVID-19 pandemic also brought about new manifestations of Münchausen syndrome, such as the simulation of long COVID, the imitation of complications after vaccination, or the creation of stories about rare side effects. This has added to diagnostic challenges, given the limited understanding of the disease and its consequences.
Cultural Aspects of the Disorder
An intriguing area of study is the exploration of cultural variations in the manifestation of Münchausen syndrome. Different cultures exhibit diverse patterns of illness simulation. For instance, in Western countries, rare autoimmune diseases and cancers are more commonly simulated, whereas in Asian countries, neurological disorders and unexplained pain syndromes are more prevalent.
Cultural context also influences societal perceptions of the disorder and, consequently, the choice of symptoms to simulate. In societies where certain illnesses are considered particularly “prestigious” or empathy-inducing, patients are more likely to select those conditions for imitation.
Gender Differences
Although historically it was believed that Münchausen syndrome is more common among men, recent studies suggest a more complex picture. Gender differences are evident not so much in the prevalence of the disorder as in the ways it is expressed. Men are more likely to simulate acute conditions requiring emergency care (heart attacks, injuries), whereas women tend to imitate chronic illnesses that require long-term treatment.
Of particular interest is the study of gender aspects in Münchausen syndrome by proxy. The predominance of mothers among perpetrators may be linked to social expectations about the maternal role as the primary caregiver and the unique formation of maternal identity in modern society.

Psychological Mechanisms and Causes of Development
Munchausen syndrome is based on a complex interplay of psychological traumas, personality development traits, and social factors. Research shows that many patients experienced various forms of abuse or neglect in childhood. Serious dysfunctions were often observed within their families, including parental mental disorders, contradictory parenting styles, emotional coldness, or, conversely, overprotection.
Early experiences with the medical system play an important role. Many patients suffered serious illnesses in childhood or witnessed the illnesses of close relatives. In these situations, they observed how illness could become a way to receive attention and care. Gradually, this developed into a stable behavior pattern, where the person cannot find another way to satisfy their emotional needs.
At the neurobiological level, patients with Munchausen syndrome exhibit certain brain functioning peculiarities. Modern studies indicate disturbances in the limbic system, responsible for emotional regulation, and an imbalance of neurotransmitters.
A particular interest lies in findings regarding dysfunctions in the brain’s reward system. Patients with Munchausen syndrome show heightened activation of this system in response to receiving attention and care in a medical context, which may explain the development of dependent behavior.
There is also evidence suggesting a possible genetic predisposition to developing this disorder, though this hypothesis requires further investigation.
The Role of Psychosocial Factors in Munchausen Syndrome Development
Munchausen syndrome is a multilayered phenomenon rooted not only in biological or psychological mechanisms but also in significant psychosocial factors. One of the key reasons for the syndrome’s development may be social isolation or a lack of emotional support from family and society.
Patients often experience feelings of loneliness, lacking genuine understanding from others, which drives them to seek attention through medical interventions. Social factors, such as dysfunctional family relationships and the persistent neglect of a child’s emotional needs, can significantly increase the risk of developing this disorder.
Munchausen syndrome may also be linked to a broader culture where attention to health and illness becomes a way to gain emotional support. In some societies, illness is associated with care, attention, and even a certain status, which creates a foundation for those who seek to use illness symptoms as a means of manipulation.
Furthermore, exposure to modern media also affects the spread and development of the syndrome. The endless flow of medical stories and articles on rare diseases can inspire people predisposed to the disorder to simulate certain symptoms to attract attention and care from others.

Diagnostic Features
Diagnosing Munchausen syndrome is a complex task for the medical community. The main difficulty is that patients actively resist detection and possess sufficient knowledge to convincingly simulate various illnesses. They may move from city to city for years, changing doctors and hospitals, which complicates the collection of a complete medical history.
The diagnostic process requires thorough medical examination and psychiatric evaluation. Physicians must rule out genuine diseases before suspecting Munchausen syndrome. At the same time, there is a risk of missing a real pathology if simulation is suspected too early. Therefore, diagnosis should be conducted with particular care and include consultations with various specialists.
It is essential to differentiate Munchausen syndrome from other conditions, such as hypochondria or somatoform disorders. In hypochondria, a person genuinely believes they have a disease and feels a real fear for their health. In the case of somatoform disorders, symptoms occur involuntarily, without the patient’s conscious involvement. Munchausen syndrome is distinct due to the intentional nature of actions in the absence of obvious external benefits.
The Role of Modern Technologies in Diagnosis
Advances in technology offer new possibilities for diagnosing Munchausen syndrome:
- Unified Electronic Medical Records:
- The ability to track medical visits across different institutions.
- Automatic detection of suspicious hospitalization patterns.
- Early warning systems for medical personnel.
- Artificial Intelligence:
- Analysis of big data to identify characteristic behavioral patterns.
- Predicting the risk of disorder development based on a set of factors.
- Assistance in differential diagnosis.

Modern Approaches to Treatment
Treating Munchausen syndrome requires a long-term and comprehensive approach. The foundation of therapy is psychotherapeutic work aimed at uncovering and addressing the deep-seated causes of the disorder. Cognitive-behavioral therapy helps patients recognize their destructive behavior patterns and find healthier ways to meet their emotional needs.
However, cognitive-behavioral therapy alone may not be enough for deep-seated changes. Emotional correction, focused on addressing childhood traumas and deficiencies in emotional development, is essential. Patients learn to express their needs and experiences without resorting to simulation or dramatization of their condition. In this aspect, psychodynamic therapy methods are often used, helping explore the unconscious motives behind pathological behavior.
In some cases, medication may be necessary, especially if the syndrome is accompanied by depression, anxiety, or other mental disorders. New-generation antidepressants, mood stabilizers, and other medications are selected individually for each patient. However, pharmacotherapy should always be combined with psychotherapeutic work.
Particular attention is given to building therapeutic relationships with the patient. Doctors and therapists must create an atmosphere of trust and safety while avoiding manipulation by the patient. This requires special professionalism and a constant balance between empathy and establishing clear boundaries.
Innovative Therapy Methods
In recent years, new approaches have emerged for treating Munchausen syndrome:
- Virtual Reality (VR) in Therapy:
- Creating a safe environment for working through traumatic experiences.
- Training in emotional regulation skills.
- Modeling social situations.
- New-Format Group Therapy:
- Peer support programs with former patients.
- Family groups for dealing with codependency.
- Specialized groups for parents of children affected by delegated Munchausen syndrome.
- Integrative Approaches:
- Combining traditional psychotherapy with telemedicine.
- Incorporating body-oriented therapy methods.
- Using art therapy and other creative methods.

Social and Economic Implications
The Munchausen syndrome has a devastating impact not only on the patient but also on their close ones. Families often face significant financial hardships due to constant medical expenses. Emotional exhaustion, loss of trust, and broken relationships are common consequences of this disorder.
The syndrome also places a considerable burden on the healthcare system. Unnecessary medical procedures, repeated hospitalizations, and examinations result in a waste of resources that could be used to help other patients.
Rehabilitation for Munchausen syndrome is a long process, requiring a gradual return to normal life. Social adaptation plays an essential role here: resuming work, re-establishing interpersonal relationships, and finding new sources of self-fulfillment. Many patients benefit from participating in support groups where they can meet people with similar experiences.
Economic Aspects
The economic damage caused by Munchausen syndrome to the healthcare system is substantial and often underestimated. According to some estimates, a single patient with this disorder may cost the healthcare system between $200,000 and $1,000,000 per year.
Indirect economic losses include:
- Time spent by medical staff
- Occupation of hospital beds
- Costs of medications and supplies
- Diagnostic procedure expenses
- Legal costs from lawsuits
- Professional burnout of healthcare personnel
Professional Burnout of Healthcare Personnel
Working with patients who have Munchausen syndrome creates a high risk of professional burnout among healthcare personnel due to:
- Constant tension from the need to verify symptom authenticity
- Emotional exhaustion from patients’ manipulative behavior
- Internal conflict between professional duty and suspicions of feigning illness
- Fear of legal repercussions for misdiagnosis
To prevent burnout and create a supportive environment for working with patients, it’s essential to implement psychological support programs for healthcare personnel. These may include regular supervision, consultations with psychologists and training on dealing with manipulative patients. Medical staff need to maintain an emotional distance while still showing empathy and respect for the patients, despite their behavior.
Emotional Consequences for Patients and Their Families
Munchausen syndrome not only disrupts the patient’s life but also has a huge impact on their family. Relatives and loved ones often become unwitting participants in dramatic episodes, constantly dealing with the patient’s complaints and claims. The emotional consequences can be devastating: close ones experience disappointment, despair, and fear for the patient’s health and well-being. Paradoxically, people with this syndrome frequently manipulate the emotions of others, provoking expressions of sympathy and care.
Children whose parents suffer from Munchausen syndrome are particularly vulnerable. In families where one parent manipulates their own or their children’s symptoms to seek attention, an unstable and traumatic environment develops, which can negatively affect the children’s psychological development. Teenagers raised in such conditions may develop distrust toward the medical system, fear of illness, or even tendencies toward similar behavioral patterns.
Legal and Ethical Aspects
Munchausen syndrome raises complex ethical and legal issues, especially in cases where patients file lawsuits against medical institutions or when it involves Munchausen syndrome by proxy.
Medical organizations face a dilemma: how to protect themselves from unfounded claims while respecting the patients’ rights to medical care. There is a need to develop clear legal protocols for such cases, balancing both the patients’ rights and the interests of healthcare institutions.
The Role of Media in Shaping the Perception of Munchausen Syndrome
The media plays an important role in shaping public opinion about various mental disorders, including Munchausen syndrome. Excessive attention to rare diseases and dramatization of cases involving simulation in popular TV shows or articles can create a false impression that such behavior is more common than it actually is. This, in turn, may influence individuals prone to simulation disorders, provoking them to imitate these symptoms.
On the other hand, the media can also help raise awareness among the public and healthcare personnel about the complexities of diagnosing Munchausen syndrome. A proper understanding of the causes and manifestations of this disorder can help doctors and society as a whole avoid stigmatizing patients, facilitating timely and adequate assistance.

Prevention and Prospects
Preventing the development of Munchausen syndrome starts with early identification of risk factors. Special attention should be given to children from disadvantaged families and those who experienced severe illnesses in childhood. Psychological education of healthcare workers plays a key role; they must be able to recognize early signs of the disorder.
Contemporary research on Munchausen syndrome focuses on several key areas. Scientists are studying its genetic and neurobiological mechanisms and developing new methods of diagnosis and therapy. Of particular interest is the investigation of the virtual form of Munchausen syndrome, which is becoming more widespread in the age of social media.
Promising Research Directions
- Genetic Research:
- Searching for genetic markers predisposing to the disorder
- Studying epigenetic mechanisms
- Examining familial cases of the disorder
- Neurobiological Research:
- Studying the role of neurotransmitter systems
- Investigating structural brain changes
- Searching for biomarkers of the disorder
- Sociological Research:
- Examining the influence of social media on manifestations of the disorder
- Studying cultural factors
- Exploring the social consequences of the disorder
Recommendations for the Medical Community
- Organizational Measures:
- Establish specialized departments for working with such patients
- Develop interdepartmental interaction protocols
- Implement early detection systems
- Educational Programs:
- Train medical personnel to recognize signs of the disorder
- Conduct training on managing complex cases
- Develop burnout prevention programs
- Informational Support:
- Create databases for sharing experiences
- Develop informational materials for patients and their families
- Organize consulting support for medical personnel

Conclusion
Munchausen syndrome is a complex disorder that requires a multi-level approach to diagnosis and treatment. Behind each case of this disorder are intricate psychological mechanisms often connected to childhood trauma and a lack of emotional support. To work effectively with these patients, it is essential not only to recognize the symptoms but also to find a balance between empathy and setting clear boundaries in the therapeutic process.
In light of modern technologies such as unified electronic medical records and artificial intelligence, new horizons are opening for a more accurate and rapid diagnosis of Munchausen syndrome. However, it is essential to understand that digitalization in medicine should be accompanied by expanded knowledge of healthcare personnel regarding psychosomatic disorders to avoid premature or erroneous conclusions.
Special attention should also be given to providing emotional support to both patients and their families. Many individuals with Munchausen syndrome require long-term psychotherapeutic help to help them recognize their destructive behavior patterns and learn to express their emotional needs in a healthy way.
Equally important is support for healthcare workers dealing with such patients. Constant emotional tension and manipulations from patients can lead to professional burnout and reduce the quality of care. It is essential to create conditions for emotional relief and train specialists in methods of dealing with challenging patients.
Finally, it is important to remember that the success of treating Munchausen syndrome depends on timely identification of the disorder and a comprehensive approach to therapy. Only a combination of psychotherapy, medical assistance, and social support can lead to successful outcomes and help patients return to normal life.