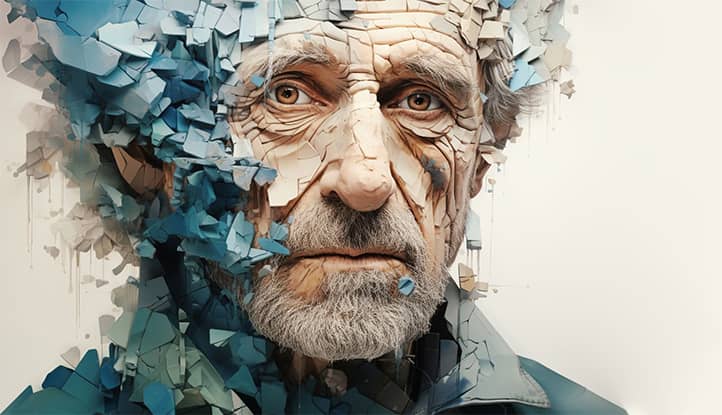
Parkinson’s disease is a progressive neurological disorder that affects movement, balance, and coordination. It impacts millions of people worldwide, and while there is no cure yet, an appropriate response to symptoms can significantly improve patients’ quality of life. In this article, I will explain how to recognize Parkinson’s disease symptoms and respond to them effectively.
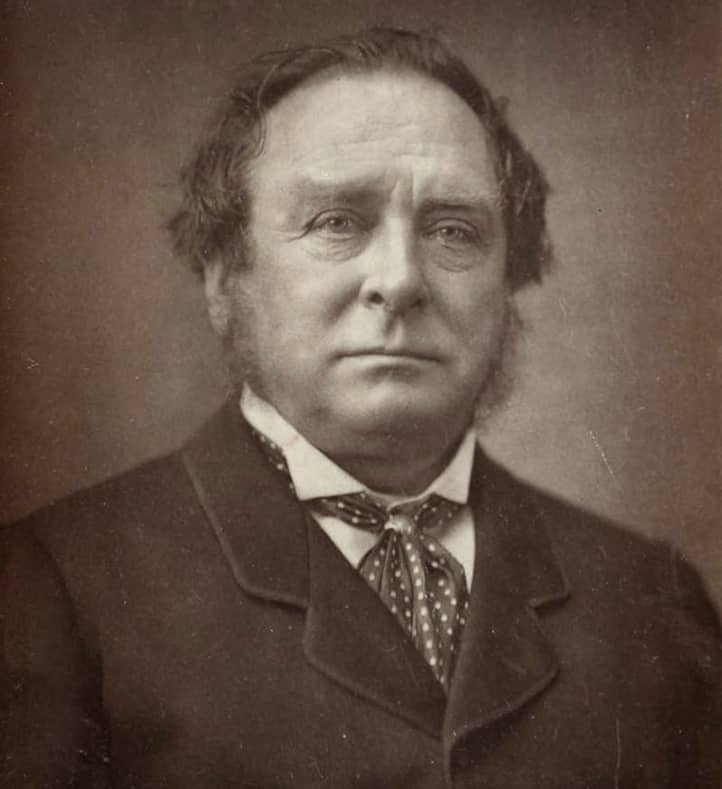
Parkinson’s disease was first described by English physician James Parkinson in 1817. Since then, our understanding of this disease has greatly improved, yet it remains one of the most common neurodegenerative disorders globally.
What is Parkinson’s Disease?
Parkinson’s disease is a chronic progressive disorder of the nervous system that primarily affects a person’s motor functions. It arises from the gradual death of neurons in a particular part of the brain called the substantia nigra. These neurons produce dopamine—a neurotransmitter that plays a key role in controlling movement.
Why is Proper Symptom Response Important?
A proper and timely response to Parkinson’s symptoms is essential for several reasons:
- Improved Quality of Life: Effectively managing symptoms allows patients to maintain independence and lead an active lifestyle for longer.
- Slowing Disease Progression: While Parkinson’s is incurable, appropriate intervention and lifestyle can slow its progression.
- Preventing Complications: Timely response to symptoms helps avoid falls, injuries, and other complications.
- Emotional Well-being: Learning to manage symptoms helps maintain a positive outlook and combat depression, which often accompanies the disease.

Primary Symptoms of Parkinson’s Disease
Parkinson’s disease is characterized by several symptoms that vary from person to person. However, there are four main symptoms that doctors consider cardinal signs of the disease. Let’s look at each in detail.
Tremor
Tremor is perhaps the most well-known symptom of Parkinson’s disease. It is characterized by involuntary rhythmic shaking of limbs, usually starting with the hands or fingers.
Characteristics of tremor in Parkinson’s disease:
- Typically starts on one side of the body.
- Most noticeable at rest.
- May intensify with stress or anxiety.
- Often described as “counting coins” or “pill-rolling.”
It is important to note that not all patients with Parkinson’s disease develop tremor, and its presence does not always indicate Parkinson’s.
Muscle Rigidity
Rigidity, or muscle stiffness, is increased muscle resistance during passive movement of a limb. This symptom may cause:
- Pain and discomfort in muscles.
- Limited range of motion.
- “Cogwheel” sensation—feeling of intermittent resistance during limb movement.
Rigidity can affect any part of the body but most commonly appears in the limbs and neck.
Bradykinesia (Slowness of Voluntary Movement)
Bradykinesia is one of the most disabling symptoms of Parkinson’s disease, manifesting as:
- Difficulty initiating movement.
- Slowed daily activities (e.g., dressing, eating).
- Reduced range of motion.
- Impaired fine motor skills (e.g., buttoning clothes, writing).
Bradykinesia may also affect facial expressions, making the face less expressive (a so-called “mask-like face”).
Postural Instability
Postural instability, or impaired balance, usually appears in later stages of Parkinson’s disease. It is characterized by:
- Difficulty maintaining balance.
- Postural issues.
- Increased risk of falls.
This symptom can be particularly dangerous as it raises the risk of injuries and fractures.

How to Respond to Motor Symptoms
Motor symptoms of Parkinson’s disease can significantly impact a patient’s daily life. However, strategies exist to effectively manage these symptoms and maintain a good quality of life.
Managing Tremor
Tremor can be one of the most noticeable and troubling symptoms. Here are some strategies that may help:
- Medication: Levodopa and other antiparkinsonian medications significantly reduce tremor.
- Deep Brain Stimulation (DBS): Some patients with severe, medication-resistant tremor may benefit from this surgical procedure.
- Relaxation Techniques: Stress can worsen tremor, so relaxation methods such as diaphragmatic breathing or meditation may be useful.
- Physical Activity: Regular exercise, especially those that improve balance and coordination, helps control tremor.
- Weighted Items: Special weighted utensils, mugs, and other objects can reduce the visibility of tremor during daily activities.
Strategies for Managing Muscle Rigidity
Muscle rigidity can cause discomfort and limit mobility. Here’s how to manage it:
- Regular Stretching: Daily stretching exercises help maintain muscle and joint flexibility.
- Physical Therapy: Working with a physical therapist can help develop a personalized exercise program to combat rigidity.
- Massage: Regular massage helps relax tense muscles and reduce pain.
- Heat Therapy: Applying heat (e.g., warm compresses or baths) helps relax muscles and decrease stiffness.
- Proper Posture and Ergonomics: Maintaining certain postures when sitting and standing, along with using ergonomic furniture, can partially relieve muscle tension.
Strategies for Improving Mobility
Bradykinesia can greatly complicate daily activities. Here are some strategies that may help:
- Physical Exercise: Regular physical activity, especially aerobic exercises and endurance training, improves overall mobility.
- Dancing: Dance-movement therapy, especially tango, has shown positive effects on mobility in Parkinson’s patients.
- Big Movements Technique: Practicing intentional, larger movements helps overcome the tendency toward reduced movement amplitude.
- External Cues: Visual or auditory cues (e.g., lines on the floor or rhythmic music) aid in initiating and maintaining movement.
- Action Planning: Breaking complex tasks into smaller steps makes them easier to accomplish.
Techniques for Maintaining Balance
Postural instability increases the risk of falls, so it’s important to focus on balance maintenance:
- Balance Training: Specific balance exercises, like standing on one leg or walking in a straight line, improve stability.
- Tai Chi: This ancient Chinese practice has proven effective in improving balance in Parkinson’s patients.
- Assistive Devices: Canes, walkers, or specialized orthopedic devices provide extra support when walking.
- Proper Footwear: Comfortable shoes with non-slip soles enhance stability.
- Home Modifications: Remove obstacles, install handrails, and use non-slip mats to reduce the risk of falls.
Remember, each patient is unique, and what works for one person may not suit another. It is essential to work with a neurologist and other specialists to develop a personalized symptom management plan.

How to Address Non-Motor Symptoms?
While motor symptoms of Parkinson’s disease are the most noticeable, non-motor symptoms have a similarly significant impact on the quality of life of patients. Recognizing these symptoms and knowing how to address them is crucial.
Cognitive Changes
Many patients with Parkinson’s disease experience cognitive issues, ranging from mild impairments to dementia.
Symptoms:
- Difficulty concentrating.
- Slowed thinking.
- Problems with planning and performing complex tasks.
- Memory issues.
How to respond:
- Regularly engage in brain exercises, such as puzzles, crosswords, or learning a new language.
- Establish and follow a clear daily routine.
- Use calendars, to-do lists, and other organizational tools.
- Stay socially engaged, as social interaction helps maintain cognitive functions.
- For significant cognitive impairments, consult a neuropsychologist for assessments and recommendations.
Emotional Issues (Depression, Anxiety)
Depression and anxiety are common in Parkinson’s disease and can severely reduce quality of life.
Symptoms:
- Persistent feelings of sadness or anxiety.
- Loss of interest in previously enjoyable activities.
- Sleep disturbances.
- Feelings of hopelessness or helplessness.
- Unfounded fears or worry.
How to respond:
- Consult a therapist or psychiatrist who specializes in working with Parkinson’s patients.
- Antidepressants or anxiolytics may be helpful, but they should be carefully chosen in consideration of the primary disease.
- Cognitive-behavioral therapy (CBT) can help modify negative thought patterns and behaviors.
- Interacting with others who live with Parkinson’s can provide significant emotional support.
- Regular physical exercise promotes endorphin production and may improve mood.
- Meditation, deep breathing, and progressive muscle relaxation help manage anxiety.
Sleep Disorders
Sleep problems are very common in Parkinson’s and may include insomnia, excessive daytime sleepiness, and REM sleep behavior disorders.
Symptoms:
- Difficulty falling or staying asleep.
- Frequent nighttime awakenings.
- Daytime sleepiness.
- Nightmares or motor activity during sleep.
How to respond:
- Stick to a regular sleep schedule, create a comfortable sleep environment, and avoid caffeine and alcohol before bed.
- Regular physical exercise improves sleep quality, but avoid intense workouts in the evening.
- Discuss with your doctor the possibility of adjusting medication timing to reduce nighttime symptoms.
- Exposure to bright light during the day helps regulate circadian rhythms.
- In some cases, sleep medications may be prescribed, but they should be used with caution.
- If sleep apnea is present, a CPAP machine may be recommended.
Autonomic Dysfunction
Parkinson’s disease can impact the autonomic nervous system, causing various autonomic disorders.
Symptoms:
- Orthostatic hypotension (dizziness upon standing).
- Constipation.
- Urinary incontinence or frequent urination.
- Excessive sweating.
- Sexual dysfunction.
How to respond:
1. Orthostatic Hypotension:
- Stand up slowly, especially in the morning.
- Increase salt and fluid intake (with physician approval).
- Wear compression stockings.
2. Constipation:
- Increase fiber and fluid intake.
- Engage in regular physical activity.
- Discuss with your doctor the use of laxatives.
3. Urinary Issues:
- Plan regular trips to the bathroom.
- Perform pelvic floor exercises.
- Consult a urologist for additional guidance.
4. Excessive Sweating:
- Wear lightweight, breathable clothing.
- Use antiperspirants.
- Avoid triggers such as spicy foods or alcohol.
5. Sexual Dysfunction:
- Discuss the issue openly with your partner and doctor.
- Consider consulting a sex therapist.
- Explore alternative forms of intimacy.
Remember that many of these non-motor symptoms may be linked not only to Parkinson’s disease itself but also to medication side effects or coexisting conditions. It’s essential to discuss any new or worsening symptoms with your doctor.
Medication Management in Parkinson’s Disease
Medication therapy plays a crucial role in managing Parkinson’s symptoms. Although medications cannot stop disease progression, they significantly improve the quality of life. Proper use and understanding of medications are critical for effective treatment.
Importance of Adhering to Medication Regimen
Following the prescribed medication schedule is crucial for controlling Parkinson’s symptoms. Here’s why this is important:
- Stable medication levels: Many Parkinson’s medications work best when their blood levels remain stable.
- Prevention of “on-off” effects: Regular medication intake helps avoid sudden fluctuations in symptom control.
- Maximizing effectiveness: Medications are most effective when taken as directed by a physician.
- Minimizing side effects: Proper medication timing reduces the likelihood or intensity of side effects.
Tips for adherence:
- Use pill organizers or reminder apps.
- Keep a diary of medication intake and symptoms.
- Discuss with your doctor the possibility of simplifying your regimen if it’s too complex.
- Always carry necessary medications when leaving the house.
Main Medication Groups
- Levodopa is the most effective drug for treating Parkinson’s. It converts into dopamine in the brain.
- Dopamine agonists mimic dopamine’s action in the brain.
- MAO-B inhibitors help block the enzyme that breaks down dopamine in the brain.
- COMT inhibitors help extend the action of levodopa.
- Anticholinergics help reduce tremors and rigidity.
- Amantadine helps reduce dyskinesias caused by levodopa.
How to Respond to Side Effects
Medications for treating Parkinson’s disease can cause various side effects. Here’s how to manage them properly:
- Do not stop taking medications on your own. Abrupt discontinuation can lead to a severe worsening of symptoms.
- Keep a journal. Record any new or worsening side effects, including the time they occur and their relation to medication intake.
- Inform your doctor. Notify your neurologist about any side effects. Often, adjusting the dose or timing can help minimize them.
- Be patient. Some side effects decrease over time as the body adjusts to the medication.
- Discuss alternatives. If the side effects are serious, discuss with your doctor the possibility of using alternative medications or treatment plans.
- Managing specific side effects:
- For nausea, take medications with a small amount of food.
- For dizziness, rise slowly, especially in the morning.
- For insomnia, discuss with your doctor the possibility of adjusting the timing of the last medication dose.
- Monitor interactions. Some medications and dietary supplements, including over-the-counter ones, can interact with Parkinson’s disease medications.
Remember, effective medication management is a process that requires constant dialogue between you and your doctor. Regular consultations and open communication will help optimize therapy.

Non-Pharmacological Methods
While pharmacological treatment plays a central role in managing Parkinson’s disease, non-pharmacological methods are also extremely important. They can significantly improve quality of life, help manage symptoms, and even slow the progression of the disease.
Physical Activity and Exercise
Regular physical activity is one of the most effective non-pharmacological treatment methods for Parkinson’s disease.
Benefits of physical activity:
- Improved mobility and flexibility.
- Strengthened muscles and bones.
- Enhanced balance and coordination.
- Reduced risk of falls.
- Improved mood and cognitive functions.
Recommended types of physical activity:
- Aerobic exercises:
- Walking.
- Swimming.
- Cycling or using a stationary bike.
- Dancing (especially tango).
- Strength training:
- Bodyweight exercises.
- Using light dumbbells or resistance bands.
- Stretching exercises:
- Yoga.
- Pilates.
- Tai Chi.
- Specific exercises for Parkinson’s disease:
- LSVT BIG – a program aimed at increasing movement amplitude.
- Balance and coordination training.
- Working with a physical therapist:
- Individually tailored exercises.
- Learning proper movement techniques.
It’s important to start with light loads and gradually increase their intensity and duration. Always consult your doctor before starting a new exercise program.
Proper Nutrition
Although there is no specific diet for Parkinson’s disease, proper nutrition can help manage symptoms and improve overall well-being.
Nutrition recommendations:
- Balanced diet:
- Include a variety of fruits and vegetables.
- Eat whole grains.
- Choose lean protein sources (fish, poultry, legumes).
- Limit saturated fats and sugars.
- Adequate fiber intake:
- Helps combat constipation, which is common in Parkinson’s disease.
- Sources: vegetables, fruits, whole grains, legumes.
- Sufficient fluid intake:
- Helps prevent dehydration and constipation.
- Drink 6-8 glasses of water a day, unless contraindicated.
- Monitor protein intake:
- Protein can affect the absorption of levodopa.
- Discuss with your doctor the optimal timing for protein consumption.
- Vitamins and minerals:
- Ensure adequate intake of vitamin D and calcium for bone health.
- Consider supplements after consulting with your doctor.
- Omega-3 fatty acids:
- May have anti-inflammatory effects.
- Sources: fatty fish, flaxseeds, walnuts.
- Antioxidants:
- Help protect brain cells from damage.
- Sources: berries, dark leafy greens, nuts.
Remember that some foods can affect the effectiveness of Parkinson’s medications. Always consult with your healthcare provider or dietitian before making significant changes to your diet.
Psychological Support
Psychological well-being plays an important role in managing Parkinson’s disease. Emotional stress can exacerbate physical symptoms, so it’s important to pay attention to mental health.
Methods of psychological support:
- Psychotherapy:
- Cognitive-behavioral therapy helps cope with depression and anxiety.
- Psychodynamic therapy helps adapt to life with a chronic illness.
- Support groups:
- Communicating with others living with Parkinson’s disease can be very helpful.
- Sharing experiences and coping strategies.
- Opportunity to receive emotional support.
- Relaxation techniques:
- Meditation.
- Progressive muscle relaxation.
- Breathing exercises.
- Art therapy:
- Drawing, sculpting, and music therapy help express emotions and reduce stress.
- Keeping a journal:
- Writing down thoughts and feelings can help cope with emotional difficulties.
- Maintaining social connections:
- Regular communication with friends and family.
- Participation in community events.
- Setting realistic goals:
- Helps maintain a sense of control and accomplishment.
- Learning stress management techniques:
- Time management.
- Problem-solving techniques.
Remember that seeking professional psychological help is not a sign of weakness but an important step in taking care of your health. Many people with Parkinson’s disease find that a combination of medication, physical activity, and psychological support yields the best results in managing the condition.

Adaptation of the Surroundings
Creating a safe and comfortable home environment plays a crucial role in the daily lives of people with Parkinson’s disease. Proper adaptation of the surroundings allows for the maintenance of independence, reduces the risk of falls, and facilitates the performance of daily tasks.
Changes in the Home to Enhance Safety
1. Lighting:
- Install bright but non-glaring lighting in all rooms.
- Use night lights to illuminate the path to the bathroom at night.
- Install light switches at the entrance to each room.
2. Floors and Stairs:
- Remove or securely fasten rugs and cords to avoid tripping.
- Install non-slip coverings on stairs.
- Mark the edges of steps with contrasting tape for better visibility.
3. Bathroom:
- Install grab bars near the toilet and in the shower/bath.
- Use non-slip mats in the tub and shower.
- Install a shower seat.
4. Kitchen:
- Place frequently used items on easily accessible shelves.
- Use lightweight and non-slip dishes.
- Consider installing appliances with automatic shut-off features.
5. Bedroom:
- Remove unnecessary furniture to facilitate movement.
- Install a bedside table for storing essentials.
- Use a bed at a comfortable height for easy getting up.
6. General Recommendations:
- Widen doorways if necessary for the use of walkers or wheelchairs.
- Install grab bars along walls in hallways.
- Ensure good ventilation throughout the house.
Use of Assistive Devices
Assistive devices can significantly ease daily life and help maintain the independence of patients with Parkinson’s disease.
1. For Mobility:
- Cane or walker to improve balance.
- Wheelchair for longer walks or when very fatigued.
- Stair lifts if living on multiple floors.
2. For Dressing:
- Button hooks for fastening buttons.
- Zipper extenders.
- Velcro shoes instead of laces.
3. For Eating:
- Utensils with thickened handles.
- Plates with high edges.
- Non-slip mats for plates.
4. For Writing and Handling Small Objects:
- Thick pens and pencils.
- Book holders.
- Magnifiers for reading.
5. For the Bathroom:
- Toilet seats with grab bars.
- Long sponges for washing the back.
- Electric toothbrushes.
6. Technological Solutions:
- Voice-controlled devices for lighting and appliances.
- Smartphone apps reminding about medication.
- Emergency call systems.
Remember that adapting the environment is an individual process. What works for one person may not work for another. It is recommended to consult with an occupational therapist who can assess your home and offer personalized solutions.
Regularly review and update adaptations as needs change. The goal is to create a safe and comfortable environment.

Support from Loved Ones
The role of family and friends in the life of a person with Parkinson’s disease cannot be overstated. Support from loved ones can significantly improve the patient’s quality of life and help them cope with the physical and emotional challenges of the disease.
Role of Family and Friends
1. Emotional Support:
- Listening and understanding the patient’s feelings.
- Encouraging a positive attitude.
- Helping to combat depression and anxiety.
2. Practical Help:
- Assisting with daily tasks (shopping, cleaning, cooking).
- Accompanying to doctor’s appointments.
- Helping with medication management.
3. Social Engagement:
- Encouraging participation in social activities.
- Organizing family gatherings and events.
- Helping maintain friendships.
4. Informational Support:
- Assisting in finding information about the disease and treatment methods.
- Participating in educational programs with the patient.
5. Physical Activity:
- Encouraging and supporting regular exercise.
- Taking walks or engaging in sports together.
6. Advocacy:
- Assisting in communication with healthcare professionals.
- Advocating for the patient’s interests in various situations.
How to Provide Help Effectively?
1. Respect Independence:
- Encourage the patient’s autonomy.
- Do not do for them what they can do themselves.
2. Be Patient:
- Give the patient enough time to complete tasks.
- Do not rush or interrupt.
3. Communicate Openly:
- Discuss problems and find joint solutions.
- Be honest about your feelings and encourage honesty in return.
4. Learn:
- Educate yourself about Parkinson’s disease and its symptoms.
- Attend educational seminars and support groups with the patient.
5. Take Care of Your Health:
- Don’t forget about your own needs.
- Regularly rest and care for your physical and emotional health.
6. Be Flexible:
- Be ready to adapt to the changing needs of the patient.
- Review and adjust plans as necessary.
7. Encourage Social Activity:
- Help the patient stay engaged in social life.
- Organize gatherings with friends and family.
8. Seek Help:
- Don’t hesitate to ask other family members or friends for help.
- Consider professional assistance if necessary.
Remember that caring for a patient with Parkinson’s disease can be emotionally and physically exhausting. It is important to take care of yourself to have the strength and energy to support your loved one. Don’t hesitate to reach out to professionals or support groups for caregivers.

When to See a Doctor?
Regular monitoring by a doctor is a key aspect of managing Parkinson’s disease. However, there are situations when it is necessary to consult a specialist outside of scheduled visits.
Signs of Deterioration
You should seek medical attention immediately if the following symptoms occur:
1. Sudden Deterioration in Mobility or Increased Tremors:
- Especially if it is not related to changes in medication regimen.
2. Appearance or Intensification of Hallucinations:
- Visual, auditory, or tactile hallucinations may be a side effect of medications or a sign of disease progression.
3. Significant Changes in Cognitive Function:
- Sudden confusion.
- Sharp decline in memory.
- Difficulty concentrating.
4. Symptoms of Depression or Anxiety:
- Persistent feelings of sadness or hopelessness.
- Loss of interest in usual activities.
- Thoughts of suicide or self-harm.
5. Balance Problems and Frequent Falls:
- Increased frequency of falls.
- Sudden deterioration in balance.
6. Changes in Medication Efficacy:
- Medications no longer work as effectively as before.
- Appearance of severe fluctuations in condition (“on-off” effect).
7. Unexpected Side Effects of Medications:
- Severe nausea or vomiting.
- Allergic reactions (rash, itching).
- Heart rhythm disturbances.
8. Problems with Swallowing or Breathing:
- Difficulty swallowing food or liquids.
- Choking or coughing while eating.
- Shortness of breath at rest.
9. Severe Pain:
- Especially if it is not related to known causes and does not respond to regular pain relievers.
10. Changes in Urination or Bowel Function:
- Incontinence.
- Severe constipation or diarrhea.
- Difficulty emptying the bladder.
Importance of Regular Consultations
Regular consultations with a neurologist specializing in Parkinson’s disease play an important role in managing the condition. Here’s why they are so important:
1. Monitoring Disease Progression:
- The doctor can assess how quickly the disease is progressing.
- This helps timely adjust the treatment plan.
2. Optimizing Medication Therapy:
- Dosages and combinations of medications may need regular adjustments.
- The doctor may suggest new drugs or treatment methods.
3. Assessing the Effectiveness of Non-Medication Methods:
- Discussion of the effectiveness of physical exercise, diet, and other strategies.
4. Early Detection of Complications:
- Some complications of Parkinson’s disease can be prevented or minimized with early detection.
5. Psychological Support:
- Regular visits provide an opportunity to discuss the emotional aspects of living with the disease.
6. Patient Awareness:
- The doctor can provide current information on new research and treatment methods.
7. Coordination of Interdisciplinary Care:
- The neurologist may refer to other specialists (physiotherapist, speech therapist, psychologist) as needed.
The recommended frequency of visits may vary depending on the stage of the disease and the individual needs of the patient. Typically, this is every 3-6 months, but it may be more frequent in the early stages of the disease or when the treatment regimen changes.
Before each visit, it is helpful to:
- Keep a diary of symptoms and side effects.
- Write down questions that arise between visits.
- Prepare a list of all medications being taken, including over-the-counter drugs and supplements.
Remember that effective management of Parkinson’s disease is a team effort between the patient, their loved ones, and healthcare professionals.

Conclusion
Living with Parkinson’s disease is challenging, but the right approach to managing symptoms and overall health can significantly improve quality of life. It is important to remember the necessity of maintaining a positive attitude. This begins with accepting the diagnosis, which is the first step towards effective disease management. Focus on the aspects of life that you can control and remember to celebrate even small achievements in managing symptoms or daily activities.
Maintaining social connections plays a key role in improving emotional well-being. Interacting with loved ones and participating in support groups has a significant positive impact. Continue to learn and discover more about the disease and its treatment methods—this will provide a sense of control and hope. Planning for the future, setting goals, and organizing activities will ensure a sense of purpose and motivation. Don’t forget to practice gratitude by reminding yourself daily of the positive aspects of life, which will improve your overall mood.
For additional information and support, there are many resources available. National and international organizations, such as the International Parkinson’s Disease Society, the European and American Parkinson’s Disease Associations, provide valuable information and support. Local support groups, which can be found through local hospitals or neurological clinics, can also be helpful. Online resources, including forums, social media groups, webinars, and online courses, offer opportunities for education and communication.
Educational materials, such as books about living with Parkinson’s disease and popular science articles on the latest research, will deepen your understanding of the condition. Specialized rehabilitation centers offer comprehensive programs for individuals with Parkinson’s disease. Many organizations also provide hotlines for information and support.
Remember that living with Parkinson’s disease is a journey, and you are not alone on this path. Millions of people around the world live with this diagnosis, and many of them lead active, fulfilling lives. With the right approach, support from loved ones, and healthcare professionals, one can effectively manage symptoms and enjoy life.
The key to success is active participation in managing your health, continuous learning, and adaptation to changes. Do not hesitate to ask questions, seek support, and try new treatment methods and strategies for symptom management. Parkinson’s disease is a challenge, but it is also an opportunity to reassess priorities, strengthen relationships with loved ones, and discover new aspects of life.
Recommended Reading
Here are some books that comprehensively cover the topic of Parkinson’s disease:
- “Parkinson’s Disease: A Complete Guide for Patients and Families” – by William J. Weiner.
This book, written by leading experts in neurology, offers a comprehensive guide for patients and their families. It addresses aspects of diagnosis, treatment, rehabilitation, and support for Parkinson’s disease. The book also highlights the latest advancements in treatment and symptom management.
- “Living with Parkinson’s Disease: A Complete Guide for Patients and Caregivers” – by Michael Okun, Irene A. Malaty, and Wissam Deeb.
This book provides a detailed overview of modern treatment methods for Parkinson’s disease, as well as tips for managing daily life. This guide is designed for both patients and their caregivers to help them better understand the condition and cope with its challenges.
- “Parkinson’s Disease: 300 Tips for Making Life Easier” – by Shelley Peterman Schwarz.
This book is a collection of practical tips aimed at improving the quality of life for people with Parkinson’s disease. The author shares experiences of adapting to changes associated with the condition, offering simple and effective solutions for everyday tasks.
- “The New Parkinson’s Disease Treatment Book: Partnering with Your Doctor to Get the Most from Your Medications” – by J. Eric Ahlskog.
This book, written by a professor of neurology, provides a detailed guide to medication therapy for Parkinson’s disease. The author explains how to work effectively with your doctor to achieve the best treatment results and discusses the latest methods and approaches to therapy.
- “Parkinson’s Disease For Dummies” – by Michele Tagliati, Gary Guten, and Jo Horne.
This book from the popular “For Dummies” series offers an accessible and comprehensive guide to Parkinson’s disease. It covers the basics of the condition, diagnosis, treatment, and support, making it an excellent resource for patients and their families.
- “Ending Parkinson’s Disease: A Prescription for Action” – by Ray Dorsey, Todd Sherer, Michael S. Okun, and Bastiaan R. Bloem.
The book offers a unique perspective on Parkinson’s disease, exploring its history, prevalence, and possible causes. The authors, leading world experts, discuss steps that can lead to the prevention and eradication of the Parkinson’s epidemic.