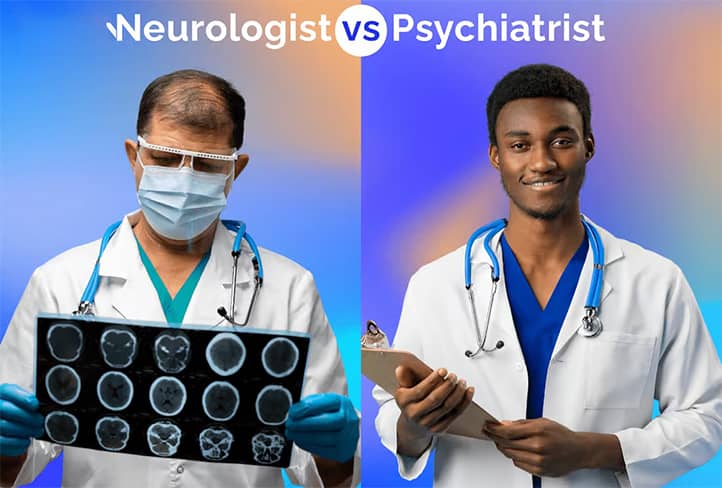
Neurology and psychiatry are two closely related medical specialties that study the brain, the nervous system, and their impact on a person’s overall condition. However, these disciplines have significant differences, which often remain unclear to patients.
People frequently confuse which specialist to visit when experiencing symptoms like headaches, insomnia, anxiety, or memory issues. This can lead to incorrect doctor selection, delays in diagnosis, and, consequently, ineffective treatment. Understanding the difference between neurology and psychiatry not only helps identify the problem correctly but also ensures timely assistance.
Moreover, many diseases overlap between physiological and psychological aspects. For example, depression may result from a neurological disorder, while chronic headaches may stem from stress or anxiety. Proper awareness of each specialist’s role ensures patients receive an effective interdisciplinary approach to treatment.
Neurology is the branch of medicine that deals with diagnosing, treating, and preventing diseases of the nervous system.
The main diseases addressed by neurology include:
- Brain diseases: strokes, migraines, tumors, Alzheimer’s disease.
- Movement disorders: Parkinson’s disease, multiple sclerosis, epilepsy.
- Nervous system injuries: consequences of traumatic brain injuries and spinal cord damage.
- Somatic disorders: weakness, numbness, seizures.
Neurologists use methods that include instrumental studies (MRI, CT, electroencephalography), laboratory tests, and clinical examination to diagnose the patient’s condition.
Psychiatry is a medical discipline specializing in diagnosing, treating, and preventing mental disorders.
The main disorders treated in psychiatry include:
- Affective disorders: depression, bipolar disorder.
- Anxiety states: panic attacks, generalized anxiety disorder, post-traumatic stress disorder (PTSD).
- Schizophrenia and psychoses: hallucinations, delusions, thought disorders.
- Personality disorders: anorexia, bulimia, addictions (alcohol, drugs, gambling).
Psychiatry methods include interviews, psychotherapy, psychopharmacological treatments (antidepressants, antipsychotics), and collaboration with other specialists, such as psychologists or neurologists.
The key difference between the two lies in their focus: a neurologist deals with physiological disorders of the nervous system, while a psychiatrist focuses on emotional and behavioral aspects, often with causes that are invisible to the eye. This makes their work complementary, yet fundamentally different.

Who Is a Neurologist?
A neurologist is a medical doctor specializing in the diagnosis, treatment, and prevention of diseases affecting the nervous system. Their work encompasses two main aspects: the central nervous system (brain and spinal cord) and the peripheral nervous system (nerves and nerve endings).
The nervous system is a complex network that coordinates the functioning of all organs and systems in the body, controlling movements, sensations, thoughts, memory, emotions, and other vital functions. Any disruption in its operation can impact a person’s quality of life, causing significant physical or emotional discomfort. Therefore, the neurologist’s role is crucial—not only in treating diseases but also in preventing their development.
The work of a neurologist often requires profound knowledge in various medical fields, including anatomy, physiology, and pharmacology, as well as the use of advanced diagnostic methods.
Specialization Description: What Are the Functions of a Neurologist?
A neurologist deals with all disorders related to the functioning of the nervous system. Their primary functions include:
- Diagnosis: Identifying the causes of a patient’s complaints through clinical examination, testing, and modern diagnostic methods (MRI, CT scans, electroencephalography).
- Treatment: Developing individualized treatment plans that may include medications, physiotherapy, or even surgical intervention.
- Prevention: Preventing the development of neurological diseases by providing lifestyle, diet, physical activity, and stress management recommendations.
- Monitoring the Patient’s Condition: Tracking disease progression, adjusting treatment plans, and preventing complications.
Neurologists work with both acute conditions (e.g., stroke, traumatic brain injuries) and chronic disorders (e.g., Parkinson’s disease, migraines). Their work often requires collaboration with other specialists, such as neurosurgeons, psychiatrists, and general practitioners.
Common Diseases Treated by Neurologists
Let’s examine the most common diseases within a neurologist’s expertise:
- Migraines: A chronic condition characterized by severe headaches lasting from several hours to several days, often accompanied by nausea, light sensitivity, and visual disturbances.
- Epilepsy: A condition where patients experience recurrent seizures due to abnormal brain activity. Neurologists determine the type of epilepsy and select treatment, which may include anticonvulsant medications.
- Stroke: An acute disruption of cerebral blood flow that can result in partial or complete loss of motor and cognitive functions. Neurologists are responsible for patient recovery post-stroke.
- Parkinson’s Disease: A neurodegenerative disorder manifesting as tremors, muscle rigidity, and coordination issues. Neurologists manage such diseases with medications to alleviate symptoms.
- Traumatic Brain and Spinal Injuries: Includes the consequences of blows, falls, and car accidents. Neurologists focus on rehabilitating patients to restore mobility and cognitive functions.
- Multiple Sclerosis: An autoimmune disease where the immune system attacks nerve fibers, leading to movement, coordination, and sensory disturbances.
- Dementia and Alzheimer’s Disease: Memory, attention, and thinking impairments that often occur in old age. Neurologists develop strategies to support such patients.
Diagnostic and Treatment Methods
Neurologists use modern methods to ensure accurate diagnosis and effective treatment:
- Clinical Examination: Includes assessment of reflexes, sensitivity, muscle strength, coordination, and balance.
- Instrumental Diagnostic Methods:
- Magnetic Resonance Imaging (MRI) and Computed Tomography (CT): To detect structural changes in the brain.
- Electroencephalography (EEG): To analyze brain activity, particularly in cases of epilepsy.
- Electromyography (EMG): To study nerves and muscles.
- Laboratory Tests: Analysis of blood and cerebrospinal fluid to detect inflammatory or autoimmune processes.
- Medication Therapy: Involves the use of drugs to relieve symptoms or treat the root cause of the disease (analgesics, anticonvulsants, antidepressants, nootropics).
- Physiotherapy and Rehabilitation: Used to restore functions after injuries or strokes.
- Surgical Intervention: In complex cases, such as tumors or hematomas, patients are referred to a neurosurgeon.
The neurologist’s work often involves not only treatment but also long-term patient management, particularly for chronic diseases. Through a comprehensive approach, neurologists help patients restore their health and return to a fulfilling life.

Who is a Psychiatrist?
A psychiatrist is a medical doctor specializing in the study, diagnosis, treatment, and prevention of mental disorders. Their work encompasses both the physiological and psychological aspects of brain and nervous system functioning, which influence emotions, thinking, behavior, and the ability to engage in social interaction.
The role of a psychiatrist goes beyond treating symptoms. They help patients gain a deeper understanding of the causes of their conditions, find ways to adapt to life challenges, and provide long-term support when necessary. Thus, psychiatry has therapeutic, rehabilitative, and preventive functions.
Mental disorders can have biological origins (e.g., hormonal imbalances, genetic factors) as well as psychological or social causes (e.g., traumatic events, stress, social isolation). Psychiatry helps balance these factors by developing an individualized approach for each patient.
Specialization Description: Focus on Mental Health and Behavioral Disorders
Psychiatry is dedicated to studying the complex processes that affect a person’s emotional and cognitive state. Psychiatrists work with:
- Emotional disorders: depression, anxiety states, panic attacks.
- Cognitive impairments: issues with memory, attention, logical thinking.
- Behavioral disorders: addictions to alcohol, drugs, gambling.
The primary goal of a psychiatrist is to understand the causes of mental health disturbances, which may stem from biological, psychological, or social factors. They use a comprehensive approach that may include psychotherapy, medication, or a combination of both.
The uniqueness of psychiatry lies in its coverage of both acute conditions (psychoses, suicidal thoughts) and chronic ones (schizophrenia, bipolar disorder).
Major Disorders Treated by Psychiatrists
Let’s take a closer look at the most common disorders within the focus of psychiatry:
- Depression. A mood disorder characterized by persistent feelings of sadness, loss of interest in life, fatigue, and changes in appetite and sleep. Psychiatrists help identify depression, determine its causes (biological or psychological), and prescribe appropriate treatment: antidepressants, psychotherapy, or a combination of both.
- Schizophrenia. A chronic mental disorder accompanied by hallucinations, delusions, disrupted thinking, and emotional disturbances. Psychiatrists work to stabilize the patient’s condition using antipsychotic medications and support their social adaptation.
- Bipolar Disorder. A disorder marked by alternating phases of depression and mania. Psychiatrists help patients manage mood swings using mood stabilizers (e.g., lithium), psychotherapy, and ongoing support.
- Anxiety Disorders. These include generalized anxiety disorder, phobias, panic attacks, and obsessive-compulsive disorder. Treatment may involve cognitive-behavioral therapy as well as prescribing anxiolytics (anti-anxiety medications).
- Addictions. States related to excessive consumption of alcohol, drugs, food, or dependence on gambling or social media. Psychiatrists analyze the causes of addiction, help overcome withdrawal symptoms, and develop strategies to prevent relapses.
Diagnostic and Treatment Methods
Psychiatrists rely on a comprehensive approach to studying and treating mental health. Key methods include:
- Patient Interviews. This is a crucial step where the psychiatrist collects the patient’s medical history, analyzes complaints, and assesses their emotional state, behavior, thinking, and speech.
- Psychodiagnostic Tests. These are used to objectively evaluate mental state, cognitive abilities, and levels of anxiety or depression. Examples: MMPI test, Beck Depression Inventory, Eysenck Personality Questionnaire.
- Psychotherapy. A treatment method based on dialogue between the patient and the doctor. Common approaches include:
- Cognitive-Behavioral Therapy (CBT): helps patients change negative thought and behavior patterns.
- Psychoanalysis: explores subconscious conflicts and traumas.
- Family Therapy: involves working with the entire family to resolve interpersonal issues.
- Medication Therapy. Prescriptions depend on the diagnosis:
- Antidepressants for treating depression and anxiety.
- Antipsychotics to manage psychosis and schizophrenia.
- Mood Stabilizers for bipolar disorder.
- Anxiolytics for panic attacks and phobias.
- Collaboration with Other Specialists.
Psychiatrists often work in conjunction with psychologists, neurologists, general practitioners, or social workers, ensuring a comprehensive approach to patient care.
By combining these methods, psychiatrists can effectively help patients improve their quality of life, stabilize their mental state, and find resources to overcome life’s challenges.
Similarities Between Neurologist and Psychiatrist
Neurology and psychiatry are medical specialties that study the functioning of the human nervous system, albeit from different perspectives. Despite their differences, they share many commonalities. Both disciplines aim to diagnose and treat disorders that affect the physical and mental health of patients.
The work of both neurologists and psychiatrists is based on a comprehensive approach to understanding the interconnections between the brain, body, and behavior. Both specialists actively use modern diagnostic and therapeutic methods to improve patients’ quality of life. They often collaborate closely, especially in cases where mental and neurological disorders are interconnected.
The complexity of the nervous system demands the integration of knowledge from various medical fields. Thus, neurology and psychiatry have many points of intersection that allow for a holistic approach to patient care.
Similarities in Diagnostic Approaches: Working with the Nervous System
Both specialists work with the nervous system, though they focus on different aspects of it:
- Neurologist examines physiological disorders affecting the brain, spinal cord, and nerves. This includes conditions such as strokes, brain injuries, epilepsy, and migraines.
- Psychiatrist focuses on mental and behavioral aspects, such as depression, anxiety disorders, schizophrenia, and bipolar disorder.
Despite their differing focuses, their diagnostic approaches share common features:
- Detailed medical history: Both neurologists and psychiatrists thoroughly analyze the patient’s medical history, complaints, lifestyle, and family health issues.
- Clinical observation: Both doctors evaluate the patient’s reactions, behavior, speech, and movements. This is essential for identifying the root causes of disorders.
- Instrumental methods:
- Neurologists use MRI, CT, and EEG to analyze the physiological state of the brain.
- Psychiatrists, though less frequently, may also employ MRI or CT to rule out organic brain lesions affecting mental health.
- Psychodiagnostic tests: Neurologists sometimes use cognitive tests to assess memory and attention, while psychiatrists use tests to determine levels of anxiety or depression.
Shared Goal: Improving the Patient’s Quality of Life
The primary goal of both neurologists and psychiatrists is to help patients return to normal life by ensuring their comfort and psychological well-being. This process involves:
- Symptom relief: Neurologists focus on alleviating physical symptoms, such as pain in migraines or muscle weakness after a stroke. Psychiatrists work on easing emotional and cognitive symptoms, such as anxiety, depression, or disorientation.
- Supporting social adaptation: Chronic neurological and mental disorders can impair a person’s ability to lead a regular life. Both specialists develop recommendations for the patient’s adaptation in society:
- Neurologists assist in restoring motor functions and improving coordination.
- Psychiatrists help maintain emotional stability and reduce anxiety in social interactions.
- Preventing relapses: Both doctors work to prevent recurrence of illnesses. For instance:
- A neurologist may recommend lifestyle changes (diet, physical activity) to prevent strokes.
- A psychiatrist develops stress management strategies to avoid depressive episodes.
- Comprehensive treatment approach: Diseases often have both physical and psychological aspects. For example, a patient with chronic pain may develop an anxiety disorder. In such cases, the neurologist and psychiatrist work together, combining their knowledge and treatment methods.
Thus, despite their different focuses, the two specialists often interact and complement each other. Neurology and psychiatry are two sides of the same coin, united by a deep understanding of the nervous system and a commitment to ensuring patients lead a high-quality life.

Differences Between Neurology and Psychiatry
Neurology and psychiatry are two interconnected fields of medicine that study the functioning of the nervous system. However, they significantly differ in their areas of focus, treatment methods, and the types of issues they address. These differences shape the uniqueness of each discipline and determine when to consult a neurologist versus a psychiatrist.
Neurology concentrates on physiological aspects: the functioning of the brain, spinal cord, nerves, and muscles. Its primary goal is to identify and treat disorders caused by organic or structural changes in the nervous system. Psychiatry, on the other hand, focuses on a person’s mental state, emotions, behavior, and thinking, exploring the psychological, social, and biological aspects of disorders.
Understanding these distinctions helps patients better determine whom to consult for assistance and fosters effective collaboration between these specialists in overlapping cases.
Object of Study: Physical Processes (Neurology) vs. Mental Processes (Psychiatry)
1. Neurology
The primary focus of neurology is physical disorders of the nervous system. Neurologists study:
- Brain diseases (strokes, tumors, injuries).
- Peripheral nervous system disorders (neuralgias, radiculitis).
- Muscle function disorders (myasthenia).
All these conditions have an organic nature, meaning they result from structural changes in tissues or disturbances in nerve pathways.
2. Psychiatry
The focus of psychiatry is mental processes and behavior. Psychiatrists study:
- Emotional disorders (depression, anxiety).
- Cognitive impairments (memory, attention).
- Social and behavioral deviations (addictions, aggression).
These disorders are often caused by a combination of biological, psychological, and social factors rather than organic damage.
Key Difference: Neurologists address the physical structure of the nervous system, while psychiatrists study the functioning of the mind and its interaction with the body.
Treatment Methods
1. Neurology Treatment Methods
Neurological treatment primarily targets physiological recovery:
- Medications: Anti-epileptics, vasodilators, anti-inflammatory drugs.
- Physiotherapy: Methods to restore nervous system function after injuries or strokes.
- Surgical interventions: Tumor removal, nerve decompression, cerebrovascular shunting.
For example, in cases of epilepsy or stroke, the primary goal is to stabilize the patient’s physical condition.
2. Psychiatry Treatment Methods
Psychiatric approaches focus on stabilizing mental health:
- Psychopharmacology: Antidepressants, mood stabilizers, antipsychotics.
- Psychotherapy: Cognitive-behavioral therapy, psychoanalysis, group therapy.
- Social rehabilitation: Helping patients reintegrate into society.
For instance, a psychiatrist might prescribe antidepressants combined with cognitive-behavioral therapy for depression.
Key Difference: Neurologists focus on organic recovery of nervous system functions, while psychiatrists emphasize correcting mental states and behavioral patterns.

When to Consult a Neurologist?
Nervous system disorders can manifest through various symptoms that are often overlooked or attributed to stress or fatigue. However, timely consultation with a neurologist can not only improve quality of life but also prevent serious complications like stroke, paralysis, or chronic pain.
Neurologists diagnose and treat disorders of the central and peripheral nervous systems affecting the brain, spinal cord, nerves, and muscles. Most neurological symptoms tend to worsen without proper treatment, making early detection crucial.
Key Symptoms
Neurological symptoms can vary depending on the type and location of the problem. Common signs indicating the need for a neurologist include:
- Persistent or severe headaches
- Migraines accompanied by nausea, sensitivity to light or noise.
- Headaches after head injuries.
- Sudden and very severe headaches, which may signal a stroke or aneurysm.
- Weakness in limbs or movement disorders
- Numbness or tingling in the arms or legs.
- Inability to lift an arm, hold an object, or walk unaided.
- Symptoms that worsen, such as loss of strength on one side of the body (possible stroke indicator).
- Seizures or involuntary muscle movements
- Repeated seizure episodes, even if brief.
- Sudden loss of consciousness with involuntary movements (potential epilepsy sign).
- Dizziness or balance issues
- Constant feeling of spinning or “rocking” sensations.
- Loss of coordination or instability while walking.
- Vision, hearing, or speech impairments
- Double vision, loss of part of the visual field.
- Hearing loss accompanied by ringing in the ears.
- Difficulty selecting words, slurred speech, or sudden loss of speech.
Symptoms can appear gradually or suddenly. In any case, their presence requires urgent consultation with a neurologist.
Complications from Delayed Consultation
Ignoring nervous system symptoms can lead to severe consequences:
- Development of chronic conditions. For example, untreated migraines can become chronic, complicating treatment and affecting quality of life.
- Deterioration of nerves and muscles. Numbness or weakness in limbs may indicate neuropathy, which progresses without treatment. In extreme cases, it can result in paralysis.
- Stroke and its consequences. Sudden headaches, limb weakness, or speech difficulties may signal a stroke. Delaying treatment even for a few hours can cause irreversible brain damage or death.
- Misdiagnosis. Some symptoms may resemble other illnesses (e.g., mental disorders). Delaying a neurologist’s consultation may result in incorrect or insufficient treatment.
- Reduced quality of life. Dizziness, headaches, or coordination issues can hinder daily activities, reducing productivity and social engagement.
Timely consultation with a neurologist not only identifies the root cause of the problem but also helps avoid serious complications. Even seemingly minor symptoms may indicate significant nervous system disorders.

When to Consult a Psychiatrist?
Mental health is an integral part of everyone’s overall well-being. However, many people ignore warning signs, attributing them to stress, fatigue, or challenging life circumstances. In some cases, these symptoms may indicate serious mental disorders that require a psychiatrist’s consultation.
Psychiatric help becomes necessary when a person’s emotional state or behavior significantly complicates their daily life. Professional intervention not only reduces symptom intensity but also prevents their progression.
Key Symptoms
Mental disorders can manifest in many forms, but there are specific symptoms that clearly indicate the need for a psychiatrist’s consultation:
1. Chronic Depression
- A persistent feeling of sadness, emptiness, or hopelessness.
- Loss of interest in favorite activities.
- Fatigue, sleep disturbances, changes in appetite.
- Thoughts of suicide or self-harm.
Depression is not just a bad mood. It’s a severe disorder that affects both physical and mental health and, without treatment, can lead to dangerous consequences.
2. Panic Attacks and Anxiety
- Sudden episodes of intense fear accompanied by rapid heartbeat, shortness of breath, sweating.
- A constant sense of anxiety or fear without an apparent reason.
- Avoidance of certain situations due to fear of a panic attack.
Panic attacks can significantly complicate life, leading to isolation and loss of social activity.
3. Hallucinations or Delusions
- Hearing voices or seeing things that don’t exist.
- Beliefs in things that aren’t real (e.g., conspiracy theories about oneself).
These symptoms may indicate schizophrenia, psychosis, or other severe mental disorders.
4. Uncontrolled Emotions and Mood Swings
- Sudden outbursts of anger, aggression, or crying.
- Sharp mood changes from euphoria to apathy.
- Feeling like emotions are “out of control.”
Such symptoms may indicate bipolar disorder or emotional regulation issues.
The Role of a Psychiatrist in Addressing Mental Health Issues
A psychiatrist plays a key role in diagnosing and treating mental disorders. Their primary responsibilities include:
1. Diagnosis. The psychiatrist begins by conducting a detailed analysis of symptoms, collecting medical history, and performing psychological tests. It’s important to identify not only obvious manifestations but also hidden causes of the disorder. For example, anxiety may be a symptom of post-traumatic stress disorder, while depression could result from hormonal imbalances.
2. Treatment Selection. Depending on the diagnosis, the psychiatrist may use:
- Medication therapy: antidepressants, anxiolytics, antipsychotics.
- Psychotherapy: cognitive-behavioral, interpersonal, group therapy.
- Family support: counseling loved ones to create a supportive environment.
3. Prevention and Long-term Support. Even after alleviating major symptoms, the psychiatrist continues to support the patient to prevent relapses. This is particularly important for patients with chronic disorders like bipolar disorder or schizophrenia.
4. Social Integration. For patients with severe mental conditions, the psychiatrist helps find ways to adapt to social life: rehabilitation programs, support groups, and self-regulation training.
Seeking help from a psychiatrist is not a sign of weakness but an important step toward preserving mental health. Symptoms that seem minor may be the early stages of a serious disorder, and only a specialist can provide appropriate help. A psychiatrist helps not only restore mental balance but also regain control over life, providing necessary support to both patients and their families.

How to Choose the Right Specialist?
Selecting the right medical professional is critical for effective treatment. Sometimes symptoms can be ambiguous, leaving a person unsure whether they need a neurologist, psychiatrist, or another doctor. A wrong choice can lead to wasted time and worsening symptoms.
To simplify the process, it’s essential to understand the primary differences between specializations, carefully evaluate your symptoms, and consult a family doctor if unsure about whom to approach. Following a step-by-step guide can help make the right and effective choice.
Step-by-step Guide: How to Determine Whom to Visit
Understanding the right specialist requires careful symptom analysis and knowledge of general medical fields. Here’s a step-by-step guide:
Step 1: Symptom Assessment
Write down all your complaints. These can be both physical symptoms (headache, numbness, weakness) and psycho-emotional ones (depression, anxiety, mood changes). Divide them into two groups:
- Physical manifestations: Likely indicate issues related to the nervous system, suggesting the need for a neurologist.
- Emotional or behavioral changes: May point to mental disorders requiring a psychiatrist’s consultation.
Step 2: Independent Research
If symptoms clearly indicate a particular issue (e.g., frequent migraines or panic attacks), familiarize yourself with the main specializations:
- Neurologist: Handles nervous system disorders like epilepsy, strokes, or neuropathies.
- Psychiatrist: Specializes in treating mental and behavioral disorders like depression, schizophrenia, and anxiety.
Step 3: Consult a Family Doctor
If symptoms seem complex or ambiguous, it’s best to start with a family doctor. They will conduct an initial assessment and refer you to the appropriate specialist.
Step 4: Choosing a Specialist
After receiving recommendations from the family doctor, select a professional based on the following criteria:
- Experience and qualifications (certificates, reviews).
- Specialization that matches your diagnosis or complaints.
- Accessibility: location, appointment schedule.

Multidisciplinary Approach
Modern medicine increasingly employs a multidisciplinary approach in diagnosing and treating complex conditions. This method is based on the collaborative work of specialists from various fields to gain a more comprehensive understanding of the problem and develop an optimal treatment plan. Collaboration between neurologists and psychiatrists serves as one of the best examples of such cooperation, as the nervous system and mental health are closely interconnected.
In many cases, diseases have both physical and psycho-emotional components. For instance, a person who has suffered a stroke may face depression, while a patient with dementia may experience both cognitive and emotional disorders. In such situations, isolated treatment does not yield the desired results, and only the teamwork of doctors enables effective therapy.
Situations Requiring Joint Work Between a Neurologist and a Psychiatrist
There are several conditions where the boundaries between neurological and mental disorders are so blurred that successful treatment is possible only when both specialists join forces:
- Dementia is a progressive disease that affects cognitive functions (memory, thinking) and is often accompanied by emotional disorders, such as anxiety or depression.
- Role of a neurologist: Diagnosis and treatment of the underlying cause of dementia (e.g., Alzheimer’s disease), control of disease progression.
- Role of a psychiatrist: Support of the patient’s psycho-emotional state, prescription of antidepressants or other psychotropic medications to reduce anxiety or aggression.
- Post-traumatic stress disorder (PTSD) often arises after physical brain injuries or emotional shocks.
- Role of a neurologist: Assessment and treatment of the physical consequences of trauma, such as impairments in brain or nerve functions.
- Role of a psychiatrist: Assistance in overcoming psychological effects through psychotherapy or medication.
- Parkinson’s disease is primarily a neurological disorder, but nearly half of the patients with this diagnosis suffer from depression or anxiety.
- Role of a neurologist: Control of motor symptoms (tremors, rigidity) and prescription of medications to improve brain function.
- Role of a psychiatrist: Treatment of depression or other psycho-emotional problems that affect the patient’s quality of life.
- Epilepsy in some patients is accompanied by mood changes, anxiety, or even psychosis.
- Role of a neurologist: Control of epileptic seizures through medications.
- Role of a psychiatrist: Stabilization of emotional state, treatment of anxiety, or psychotic episodes.
The Importance of Comprehensive Treatment
A comprehensive approach in medicine allows for consideration of all aspects of a patient’s condition—physical, mental, and emotional. Here is why it is so important:
- Holistic understanding of the disease. A neurologist and psychiatrist working together share their perspectives and expertise, enabling precise diagnosis and personalized treatment. For example, a patient with headaches and emotional instability may have both a physical issue (neuralgia) and a psychosomatic component.
- Improvement of the patient’s quality of life. Combining physical and psycho-emotional therapy not only alleviates symptoms but also helps restore a person to normal life. For instance, in dementia, treatment should aim not only to slow cognitive decline but also to support the emotional well-being of the patient and their family.
- Reduction of complications risk. In many cases, timely collaboration between a neurologist and psychiatrist prevents disease progression or the development of comorbid disorders. For example, in depression associated with Parkinson’s disease, timely psychiatric intervention prevents social isolation and deterioration of the condition.
- Psychological support for the patient. Diseases requiring a multidisciplinary approach often cause stress, anxiety, or even despair in patients. Having a team of doctors working cohesively creates a sense of care and confidence.

Conclusions
Neurology and psychiatry are two interrelated yet distinct branches of medicine, each playing an important role in maintaining human health. Neurologists focus on the physical aspects of the nervous system’s functioning, while psychiatrists deal with mental processes and behavioral disorders. Together, they provide a comprehensive approach to diagnosing and treating many complex conditions that affect patients’ quality of life.
Understanding the role of each of these specialists helps individuals better navigate their healthcare choices. Headaches, limb weakness, or dizziness are symptoms indicating the need to consult a neurologist. Conversely, depression, anxiety, or emotional instability signal the need for a psychiatrist’s consultation. In many cases, timely referral to one of these specialists not only improves quality of life but also prevents serious complications.
It is especially important to recognize that ignoring symptoms or self-diagnosis can lead to the loss of valuable time. This impacts not only the effectiveness of treatment but also the possibility of full recovery. Therefore, seeking medical advice at the first alarming signs is the best step toward preserving physical and mental well-being.